
What is IBD?
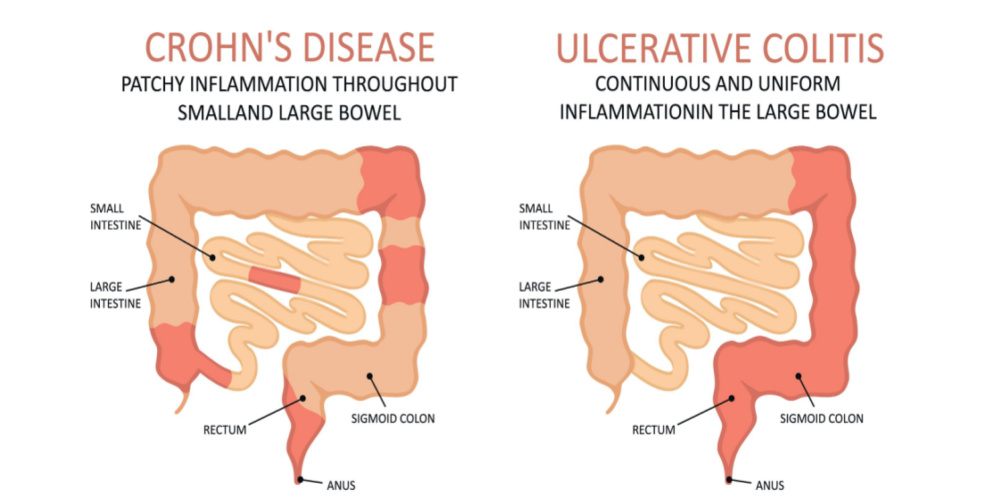
The 2 main types of inflammatory bowel diseases are Crohn’s Disease and Ulcerative Colitis. Crohn’s disease can lead to inflammation anywhere along the digestive tract whereas Ulcerative Colitis involves inflammation in the large intestine.
Multiple factors are understood to underly the onset of this inflammation and damage in the digestive tract. These include:
- Bacterial changes
- Alterations in the immune system
- Genetic factors
While genetic factors may predispose an individual to increased inflammatory response, a key influence on disease onset is more environmental in nature. This is supported by research that suggests autoimmune conditions are more prevalent in industrialised nations.
Studies have also indicated that certain dietary patterns, commonly undertaken in industrialised nations increase the risk of developing IBD.
These include the increased intake of:
Reduced intake of
- Dietary fibre [Source: Pubmed]
What are the symptoms of IBD?
The symptoms of IBD vary between the subtypes of inflammatory bowel disease and also the severity of the symptoms experienced.
While these 2 types of IBD share common aspects, there are differences between the types of gut symptoms that are seen.
The main distinction is that Crohn’s disease can impact any region of the digestive tract while Ulcerative colitis only impacts the large intestine. Additionally, in Crohn’s disease, the damage affects the entire gut wall while in Ulcerative Colitis it’s only the top layer known as the epithelium.
Another key difference is that those with Ulcerative Colitis may experience more pain in the lower left region of the abdomen where as the pain is commonly seen in Crohn’s disease is in the lower right of the abdomen.
It is also more common for those with Ulcerative Colitis to experience rectal bleed than those with Crohn’s Disease. [Source: Pubmed]
The differences between Crohn’s Disease and Ulcerative Colitis symptoms are shown in the following table:
| Key Features | Crohn’s Disease | Ulcerative Colitis |
| Location | ||
| – Upper parts of gut | Rarely | Never |
| – Distal ileum | Very common | Never |
| – Colon | Common | Always |
| – Rectum | Rarely | Never |
| Signs and symptoms | Pain in the lower right abdomen Swelling Thickening of the bowel wall | Pain in the lower left abdomen Diarrhoea Weight loss Rectal bleeding |
Is Crohn’s Disease Dangerous?
A common complication of Crohn’s disease a blockage of the bowel. The swelling of the wall of the intestines due to inflammation or fibrosis.
Due to the impact of Crohn’s disease on the small bowel, the site of absorption of vitamins and minerals, malnutrition is also common. [Source: Pubmed]
What causes IBD?
The use of antibiotics has been associated with an increased risk of IBD onset. A 2020 study founds that those with 3 or more previous antibiotics treatments had an increased risk of IBD development of 55% when compared to those with no history of antibiotics use.
This risk as higher for the development of Crohn’s Disease than it was for Ulcerative Colitis. [Source: Pubmed]
Supplements for Inflammatory bowel disease
Supplements that support anti-inflammatory processes are also central to any approach for inflammatory bowel diseases.
Due to the potential side effects of medications, these may be better tolerated.
Side effects are pharmaceutical anti-inflammatories may include vomiting, diarrhoea, and nausea. [Source: Pubmed]
Turmeric for Inflammatory bowel disease
Turmeric is often suggested in the form of curcumin.
This has a number of benefits in the gut of those with IBD. These include:
- A beneficial effects on the microbiome
- Antimicrobial properties
- Inhibition of inflammation
- Support the immune system [Source: Pubmed]
Curcumin has been studied in those with Crohn’s disease which lead to a significant improvement in symptoms are well as endoscopic findings. [Source: Pubmed]
Curcumin has also been studied alongside the IBD medications mesalamine. A review of several studies concluded that taking curcumin alongside the medication lead to an improved outcome when compared to only taking mesalamine. [Source: Pubmed]
Probiotic for Inflammatory bowel disease
One aspect of IBD onset is there is commonly an imbalance in the gut bacteria. This general balance in the microbial ecosystem is commonly referred to as dysbiosis.
It is commonly characterised by:
- Reduced microbial diversity
- Reduced levels of beneficial bacteria such as bifidobacterium and lactobacillus
- Reduced abundance of short-chain fatty acids (SCFAs) producers
- Increase levels of pro-inflammatory microbes (eg adherent/invasive E. coli and hydrogen sulphide producers)
This general imbalance also has the potential to influence the inflammation in the gut. This is understood to be via its impact on the immune system or via a metabolic pathway. [Source: Frontier, Pubmed]
Probiotics are described as beneficial bacteria that when taken in adequate amounts have a beneficial impact on the host.
In IBD, these benefits have been indicated to include:
- Inhibiting the growth of potentially harmful microbes
- Supporting the strength of the gut lining
- Supporting the immune system
- Secreting antimicrobial products
- Decomposing luminal pathogenic antigens [Source: Pubmed]
Vitamin D in Inflammatory Bowel Disease
Vitamin D plays a role in many areas of health. In the digestive tract the role of vitamin D includes:
- Supporting the integrity of the gut lining
- Supporting the immune system
- Supporting the gut microbiome
Vitamin D deficiency is more common among those with IBD than in healthy controls. Studies have found that normalizing levels of vitamin D provide benefits such as:
- Reduced risk of surgery in those with Crohn’s Disease
- Reduction in inflammatory markers
- Reduction in the development of anaemia
- Improved response to anti-TNF alpha medication treatment
- A reduction in the risk of colorectal cancer [Source: Pubmed]
Conclusion
Although there is no cure for inflammatory bowel diseases, there are key interventions to support and maintain remission.
These involve dietary, supplementation and lifestyle interventions. At the IBS & Gut Health Clinic, research into these key natural interventions is used to create personalised health plans to support your gut health with the aim of achieving and maintaining remission.






