Those who COVID-19 has infected are at an increased risk of long-term respiratory issues.
However, there may also be an impact on the digestive system.
It is well understood that digestive issues can appear following acute infectious gastroenteritis. These are symptoms such as:
- Bloating
- Cramping
- Nausea
- Constipation
- Diarrhoea
When symptoms appear after an infection, it is given a specific name. Post-infectious gastrointestinal disorders (PI-FGD) is a general term that’s used. This can cover symptoms that can be described as IBS symptoms as individual symptoms such as bloating or diarrhoea.
The reason bloating by itself is not classed as IBS is that additional factors such as pain or a change in bowel pattern also need to be present for the diagnosis of IBS to be given. [Source: Pubmed]
These gut issues are understood to develop after an infection of the digestive tract. This can be from a bacterial protozoal or viral infection.
In addition to being infected, other factors may contribute to the development of post-infectious functional gastrointestinal disorders.
These include:
- The severity and duration of the illness
- History of antibiotic use
- Female gender
- Younger age
Additionally, anxiety and depression are also seen as risk factors for digestive issues.
Due to the increased stress and worry during the pandemic, this may be a key component of symptom development. [Source: Pubmed]
IBS During COVID
A wide range of digestive symptoms are common during the acute phase of a COVID-19 infection.
These include:
- Nausea
- Vomiting
- Loss of appetite
- Abdominal pain and discomfort
- Diarrhoea [Source: Pubmed]
Specific changes have been documented to take place within the digestive tract during a COVID infection.
These include:
- An elevated level of calprotectin (indicating inflammation)
- Gut microbiome dysbiosis (imbalanced gut bacteria)
- Altered intestinal permeability (leaky gut)
The main digestive symptoms in those infected with COVID-19 are diarrhoea and vomiting. [Source: Pubmed]
COVID and Gut Health
Post-infectious digestive issues are more common following a case of viral gastroenteritis. This is reported to be 12.5% of those with viral gastroenteritis going on to develop long-term digestive symptoms.
COVID-19 is primarily a pathogen that impacts the health of the respiratory system. However, research has indicated that it can infect the digestive tract in half of those infected with the virus.
Due to only approximately 50% of those with COVID experiencing digestive issues, this supports the number of 5.3% of COVID patients developing longer-term digestive symptoms in the form of IBS. [Source: Pubmed]
IBS After COVID
A key factor that increases the risk of developing long-term gut issues following COVID-19 is the presence of digestive symptoms during the acute phase of infection with COVID-19.
This means that if symptoms are present during the infection, the risk is higher that they’ll persist.
It has also been noted that those with diarrhoea have higher levels of calprotectin (a marker of inflammation) in their stool and an increase in serotonin (which regulates muscle function) in the gut wall. This suggests that inflammatory response in the gut lining as being a possible mechanism for looser bowel movements. [Source: Pubmed]
Inflammation in the gut caused by an invading pathogen is a well-documented predictor of post-infectious digestive issues. Following COVID, this ongoing response has been seen in the lungs, and some researchers have stated that gut inflammation is not unexpected in patients with COVID-19. [Source: Pubmed]
The long-term impact and severity of digestive issues following COVID is also related to the severity of diarrhoea during the acute infection.
This suggests that the severity of symptoms relates to the injury to the gut. [Source: Pubmed]
This was indicated in research into post-infectious IBS that was carried out before the emergence of COVID-19.
This concluded that the following 3 factors:
- The severity of the injury to the gut
- The degree of inflammation
- The psychological issues (gut-brain imbalance) that present and are potentially due to the unpleasant and distressing nature of digestive issues
These may then contribute to the ongoing inflammatory response and persistent symptoms. [Source: Pubmed]
Indigestion and COVID
Indigestion, often referred to as dyspepsia, includes a range of symptoms. These include:
- Bloating
- Discomfort
- Heartburn
- Belching
During the 30 days following a COVID infection, the rates of IBS and dyspepsia seem to be similar.
However, when looked at over a 6-month period, the symptoms of dyspepsia are more likely to resolve, while IBS symptoms may continue.
This suggests different mechanisms being the symptoms of dyspepsia and IBS. Dyspepsia may be related to the systemic COVID-19 infection, while the IBS-type symptoms are due to the ongoing inflammatory response and associated changes in the gut.
The changes include:
- Microbiome dysbiosis (bacteria changes in the gut)
- Increased sensitivity of the gut lining
- Gut-brain dysregulation. [Source: Pubmed]
Long COVID and Loss of Smell and Taste
Loss of smell and taste as 2 common symptoms of the acute infection of COVID-19, which may persist following the infection.
Research carried out via autopsy on individuals with fatal COVID-19 indicated the inflammation of the central nervous system. Due to the nervous system’s role in communicating smell and taste sensations, here is a clear link to the reason for the loss of these senses.
This also indicated that specific brain regions might experience ongoing inflammation, which may then influence the gut-brain axis. Here, rather than inflammation in the gut resulting in ongoing symptoms of IBS, inflammation in regions of the brain that regulate gut function may contribute to a dysfunctional gut and digestive symptoms. [Source: Pubmed]
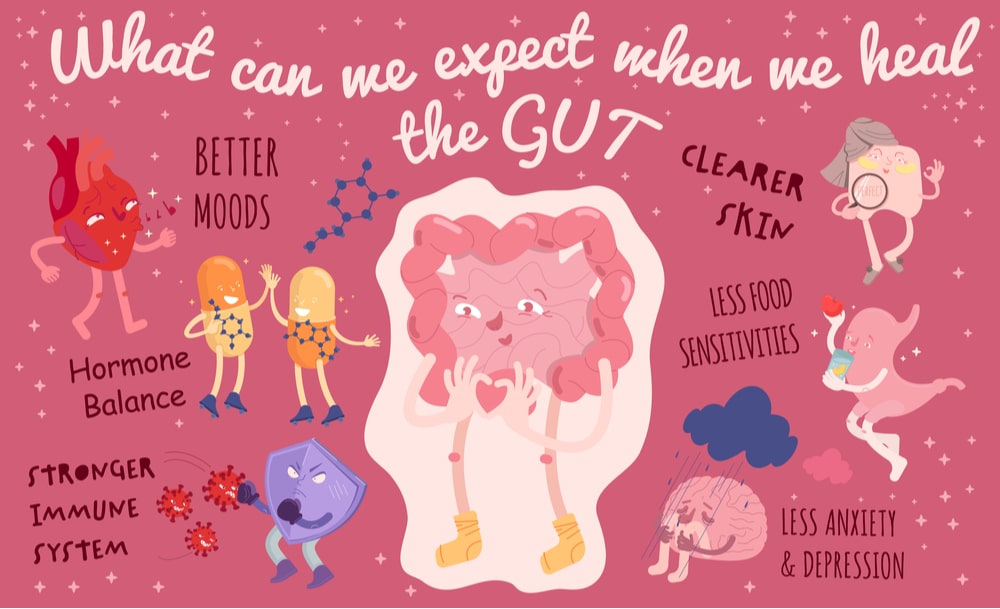
How to Address Gut Issues following COVID
Even though COVID-19 is a recent viral infection, research into the impact of post-infectious digestive issues is well established.
This means that a number of the strategies that can be considered for post-infectious IBS can also be considered for digestive symptoms that have followed a COVID-19 infection.
These include:
- Dietary modifications
- Targeted supplementation
- Lifestyle support
Dietary approaches to digestive issues involve 2 key factors. Firstly, the diversity and the fibre content of the diet promote a healthy gut microbiome and a balanced immune response in the gut. This would be working toward what is termed the Mediterranean diet.
This is a diet rich in fruits, vegetables, herbs, and spices with moderate consumption of animal products such as meat and eggs. [Source: Pubmed]
The second part of the approach may be to limit certain foods in the short term to assess for sensitivities.
This is due to the imbalances in the gut or increased sensitivity in the gut lining leading to food reactions.
A dietary approach that can be considered here is the Low FODMAP diet. This is a short-term diet that assesses for reactions to certain carbohydrates found in a wide range of foods.
Common high FODMAP foods that those with IBS react to include:
- Apples
- Garlic
- Pears
- Wheat
- Onions
Even though these foods are considered healthy, they may lead to a reaction and increase symptoms such as bloating if someone has IBS. While often helpful for managing symptoms, a downside of the diet is that it can be overly restrictive, limit lots of healthy foods and contribute to food anxiety.
The aim is to address the underlying issue, so these foods (if they are an issue) can be reintroduced. [Source: Pubmed]
Specific supplements have been well researched for the use of IBS as well as post-infectious IBS.
These include probiotics, herbal preparations, and support for the lining of the digestive system, such as glutamine. [Source: Pubmed, Pubmed]
Lifestyle support due to the role of the gut-brain connection and the vagus nerve supporting the stress response can be a central factor when addressing digestive issues.
Additionally, other factors such as sleep support and food timing are key to assess and support. These further support the function and resilience of the digestive system. [Source: Pubmed]
Conclusion
As discussed, even though COVID-19 is a virus that has only recently emerged, many reasons why it may contribute to digestive symptoms are understood.
Due to research into viral gastroenteritis, the long-term impact of a gastric infection has been well documented, along which the mechanisms outlined. In particular, how they can contribute to and result in ongoing symptoms of IBS.
Addressing the underlying factors is key when working to address symptoms of IBS and restore digestive health.