
The low FODMAP diet is a well-researched approach to help identify food triggers, most commonly in those with IBS.
This diet is structured in a way where food triggers are identified to reduce symptoms and improve quality of life.
This diet is best carried out under the care of a qualified practitioner to support and guide the process. However, it is possible to follow this diet without professional support.
This article will review the diet and ways it can be implemented.
What is a FODMAP?
FODMAPs are various types of carbohydrates naturally found in a wide range of foods.
The carbohydrates are either sugars or fibres which are generally well tolerated and considered healthy for the general population. They can also support the health of the gut microbiome.
These sugars include fructose and lactose, with the fibres including oligosaccharides. Fructose is found in high amounts in apples and pears; lactose is found in dairy products. Whereas the dietary fibres in the form of oligosaccharides are in foods that range from garlic to wheat.
How does the FODMAP diet work?
Due to underlying imbalances or irritations in the digestive system, the ability to tolerate certain foods can change.
Food intolerances are not uncommon, as 70% of those with IBS report that food is a trigger for their symptoms. However, many of these people may not know exactly what their triggers are.
While FODMAP-containing foods are considered healthy, an underlying issue in the gut can lead to symptoms. For example, a change in the balance of the gut microbiome in the small intestine may lead to fructose intolerance, a prevalent FODMAP.
The Low FODMAP diet can be considered as a dietary strategy to identify food triggers. The aim of this is to provide a clear understanding of how much these foods are contributing to symptoms.[1]
When do you need a low FODMAP diet?
A low FODMAP diet can be implemented in several situations. These can be to help calm a range of gut health and digestive symptoms.
Often this can be as a starting point where there is uncertainty around dietary triggers. It can also be if there is a flare-up in symptoms and a reset of sorts is needed.
If you have IBS
Studies have found that up to 86% of those with IBS respond positively to a low FODMAP diet. This can be seen in the improvement of a wide range of symptoms that include bloating, abdominal pain and changes in bowel functions. [2]
If you have bloating
For some individuals with digestive issues, they do not meet all of the criteria for an IBS diagnosis but only experience bloating.
This increase in gas may still be due to the same underlying issues in the gut, for example, changes in the balance of the gut microbiome. This underlying factor may then lead to reactions to FODMAP-containing foods. [3]
If you have diarrhoea
In a similar way to bloating, diarrhoea can be present as a stand-alone symptom. Without symptoms of bloating or pain, this would be referred to as functional diarrhoea and not IBS.
A possible cause of this is a food intolerance, which may be a FODMAP. Commonly, this can be due to the poor absorption of sugar (such as fructose or lactose) in the small intestine, which may then lead to a loose bowel movement.
If you have histamine intolerance
While there may still be histamine-containing foods permitted on the low FODMAP diet, a low FODMAP diet has been found to reduce the levels of histamine by 8 times. The Low FODMAP diet may be an easier diet to follow than a low histamine diet making it a good option for those with histamine intolerance. Symptoms of elevated histamine can include hives, itching, brain fog and anxiety. [4]
Benefits of the diet
The primary benefit of a low FODMAP diet is to identify dietary triggers to improve digestive symptoms and the quality of life of the patient. This can be a short-term approach while further support is in place to address the cause of the FODMAP food reactions and intolerances.
While this is often referred to as a symptom-management diet, as mentioned are also studies highlighting its effect on reducing histamine levels. As elevated histamine levels
can be used as an indication of immune activity in the gut, a low FODMAP diet may calm an immune response via lowering histamine levels. [4]
Foods high in FODMAPS
FODMAPs are found in a wide range of seemingly unrelated foods. These include:
· Fruits: High FODMAP fruits include apples, pears, mangoes, cherries, and dried fruit. · Vegetables: High FODMAP vegetables include garlic, onion, cauliflower, leeks, and mushrooms
· Grains and cereals: High FODMAP grains and cereals include wheat and rye.
· Legumes: High FODMAP legumes include beans, lentils, and chickpeas
· High-lactose dairy: High-lactose dairy foods include soft cheeses and milk
· High lactose nuts: High lactose nuts include pistachios and cashews
· Sugars and Sweeteners: FODMAPs can also be found in common sugar-sweetened foods and drinks. These are often in the form of fructose and sugar polyols (sorbitol, xylitol, erythritol) [5]
What can you eat on a low FODMAP diet?
A wide range of foods are permitted during the elimination phase of the low FODMAP diet.
These include:
· Fruits: Low FODMAP fruits include kiwi, strawberry, lime, lemon, raspberry, and pineapple.
· Vegetables: Low FODMAP vegetables include rocket, bean sprouts, bok choy, tomato, turnips, and carrots.
· Grains and cereals: Low FODMAP grains and cereals include oats, buckwheat, and rice.
· Low lactose dairy: Low lactose dairy foods include hard cheeses such as cheddar, camembert, and brie
How to follow a low FODMAP diet
Even though the list of FODMAP-containing foods is long, it’s uncommon for all of these foods to be an issue.
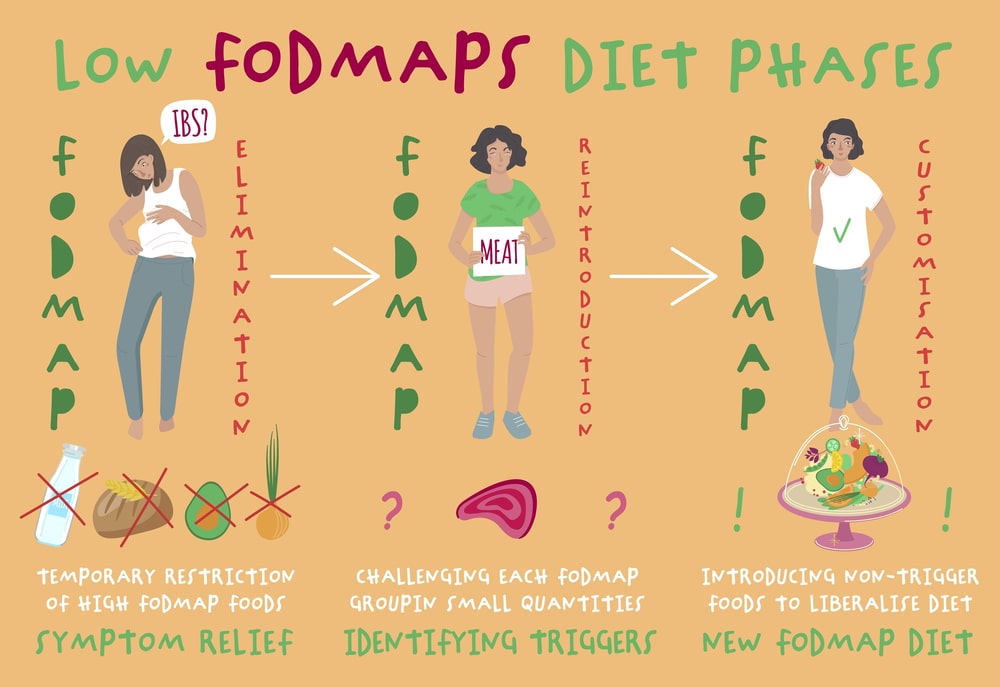
However, to identify specific triggers, the diet begins with an elimination phase with 2 further phases following this.
Name | Purpose | Duration |
Phase 1 - Elimination Phase | The strictest phase of the diet to remove all potential FODMAP culprits. | 2-6 weeks |
Phase 2 - Reintroduction Phase | The previously restricted foods are reintroduced in a specific order to assess for triggers. | 4-8 weeks |
Phase 3 - Personalisation | Often seen as a long-term strategy where the offending foods are avoided. | Discussed below |
How long is low FODMAP for?
When used in isolation, phase 3 of the low FODMAP diet is considered a long-term approach.
In simplest terms, this involved identifying the specific foods that trigger symptoms and avoiding them forever.
The problem that some have with this approach is that it does not address the reason why the reaction may be taking place. For example, you may be reacting to garlic, but why is this reaction taking place?
If FODMAP triggers are identified, their removal is primarily for symptom management and not a treatment.
This focus on food being the cause of symptoms (rather than aggravating an underlying issue) can lead to people becoming hyper-focused on their diet. This has led some to comment that a low FODMAP diet should not be considered in those with current or historical eating disorders.
The reduction in fermentation also impacts the growth of beneficial bacteria in the gut. Research indicates that key, friendly bacteria such as Bifidobacterium and Faecalibacterium prausnitzii are reduced in number in those on a low FODMAP diet.
Due to these potentially negative aspects of the low FODMAP diet, it is not considered a long-term approach. [7]
Conclusion
While a low FODMAP diet can help reduce symptoms of IBS, it doesn’t address the underlying imbalance.
Rather than asking ‘what food is causing symptoms?’ we ask, ‘why is the body reacting to food in that way?’ By addressing this underlying issue, the aim is to move towards an unrestricted diet while remaining symptom-free.
The factors that can lead to FODMAP intolerance include:
· Motility changes
· Visceral hypersensitivity (increased sensitivity of the nerves in the gut)
· Low-grade inflammation (which can follow food poisoning or a viral infection)
· Altered microbiota (imbalances in the gut bacteria)
There are also several approaches have been shown to have a similar or increased level of benefit to a low FODMAP diet. These have shown to be beneficial even without restricting FODMAP-containing foods.
· Probiotic supplementation
· Prebiotic supplementation
· Yoga and meditation
· Gut directed hypnotherapy
With the overlapping causing of digestive symptoms, an approach that combines these factors may be most effective. Working with a registered nutritionist therapist can guide the low FODMAP diet as well as work to address the underlying issue
References
- Böhn L, Störsrud S, Simrén M. Nutrient intake in patients with irritable bowel syndrome compared with the general population. Neurogastroenterol Motil. 2013 Jan;25(1):23-30.e1. doi: 10.1111/nmo.12001. Epub 2012 Sep 2. PMID: 22937900.
- Liu J, Chey WD, Haller E, Eswaran S. Low-FODMAP Diet for Irritable Bowel Syndrome: What We Know and What We Have Yet to Learn. Annu Rev Med. 2020 Jan 27;71:303-314. doi: 10.1146/annurev-med-050218-013625. PMID: 31986083.
- Pessarelli T, Sorge A, Elli L, Costantino A. The low-FODMAP diet and the gluten-free diet in the management of functional abdominal bloating and distension. Front Nutr. 2022 Nov 8;9:1007716. doi: 10.3389/fnut.2022.1007716. PMID: 36424920; PMCID: PMC9678936.
- McIntosh K, Reed DE, Schneider T, Dang F, Keshteli AH, De Palma G, Madsen K, Bercik P, Vanner S. FODMAPs alter symptoms and the metabolome of patients with IBS: a randomised controlled trial. Gut. 2017 Jul;66(7):1241-1251. doi: 10.1136/gutjnl-2015-311339. Epub 2016 Mar 14. Erratum in: Gut. 2019 Jul;68(7):1342. doi: 10.1136/gutjnl-2015-311339corr1. PMID: 26976734.
- Monash University
- Staudacher HM, Lomer MC, Anderson JL, Barrett JS, Muir JG, Irving PM, Whelan K. Fermentable carbohydrate restriction reduces luminal bifidobacteria and gastrointestinal symptoms in patients with irritable bowel syndrome. J Nutr. 2012 Aug;142(8):1510-8. doi: 10.3945/jn.112.159285. Epub 2012 Jun 27. PMID: 22739368.
History
- Updated 19/09/24 by Martin Cohen.






