Most of the people that we see in the clinic have IBS (irritable bowel syndrome). They’ve been told by their well-meaning Doctor or health care provider to self-manage the IBS condition but only provided with basic health information as an IBS patient. This can involve guidance to avoid IBS triggers but the reality is that the triggers are rarely known. It can be especially confusing when the healthier the food on the plate, the worse the IBS symptoms of bloating, constipation and abdominal pain. It’s common that IBS does this.
It can also be frustrating when a doctor says that there is currently no cure for IBS.
While mild symptoms can often be controlled or cured with small changes to the diet, there is a great deal that can be done to fully resolve lower-level symptoms as well as more severe forms of IBS.
IBS impacts the lives of around 17% of the UK population. A higher percentage is actually seen in women than in men. This, however, might be the result of women being more likely to seek help for their symptoms.
Most people with IBS say it’s having a significant impact on their quality of life, mental health, as well as their social life. Although, it’s not seen to increase the risk of other serious diseases those with IBS may be at greater risk of surgical procedures such as hysterectomy and cholecystectomy. It also plays a role in being one of the main reasons for people taking time off work.
The bloating, altered bowel habits, abdominal pain, and anxiety that can come along with these symptoms can be truly debilitating.
But is IBS a real diagnosis? And how do we get the right information to address IBS?
Diagnosis of IBS
IBS (irritable bowel syndrome) will be diagnosed by the Rome IV criteria which directly relate to digestive symptoms but goes no further into investigating what could be the cause. Bloating, constipation, altered bowel habits, abdominal pain, they all tell us how we might be feeling but now why.
Once more serious digestive issues have been ruled out then IBS is often diagnosed. This leads some to believe that IBS is the lack of a diagnosis rather than a diagnosis in itself.
In reality, a wide range of factors can be contributing to the symptoms.
We can think of IBS as an umbrella term that covers the symptoms. The discomfort, constipation and abdominal pain and perhaps even the anxiety that often comes with digestive issues.
Many people reach my clinic when feel they feel they’ve come to the end of the road after being told to self-manage their symptoms but today we know a lot more about what contributes to IBS than we did even 12 months ago.
Testing For IBS
If a doctor suspects that irritable bowel syndrome is present, then further gut health tests will often be offered to rule out other causes of IBS.
These may be initial blood tests for levels of inflammation (which will help to differentiate between IBS and IBD) as well as to rule out other gut conditions such as coeliac disease.
The NICE guidelines within the UK do state that further tests are not nessesearcy to diagnose IBS.
These include:
- ultrasound
- rigid or flexible sigmoidoscopy
- colonoscopy or barium enema
There will however be a referral to a specialist if other symptoms are present. These symptoms can include:
- unintentional and unexplained weight loss
- bleeding from the rectum
- a family history of bowel or ovarian cancer.
Additionally, in the over 60’s, a sudden change in bowel patterns (constipation or diarrhoea) lasting for over 6 weeks. These factors will then influence the decision to see a specialist and further tests. [Source: NICE]
Can IBS Be Cured?
When we talk about gut health and the symptoms, we may be experiencing it’s important to remember that IBS isn’t a condition like diabetes or heart disease. In these conditions, there is a clear understanding of how they develop and how to test for them. In IBS things are less clear.
IBS is diagnosed on symptoms alone. The presence of bloating, cramping and altered stool patterns tell us a lot about how we’re feeling. However, they rarely get us any closer to understanding why we are experiencing them and more importantly what to do about them.
This ‘why‘ can be different for each individual but by understanding the gut we can work through the possible reasons and help to bring things back into balance. This means that there’s no single diet or medicine that works for everyone with IBS.
However, to cure IBS the underlying cause needs to be addressed.
Underlying causes of IBS
The multiple factors that contribute to irritable bowel syndrome have recently been explored in a peer-reviewed article entitled “Does Irritable Bowel Syndrome Exist? Identifiable and Treatable Causes of Associated Symptoms Suggest It May Not”.
This title is not suggesting that IBS is made up in our heads but it focuses on the fact that there can be many issues that combine to contribute to the gut being sent out of balance.
When things go out of balance there is disruption, and this is what is leading to the symptoms.
So, in order to ‘cure’ IBS, it’s vital to identify which issues are most relevant to each person and their individual version of IBS. It’s by addressing these underlying issues that we can bring the gut back into balance.
Root causes of IBS (irritable bowel syndrome)
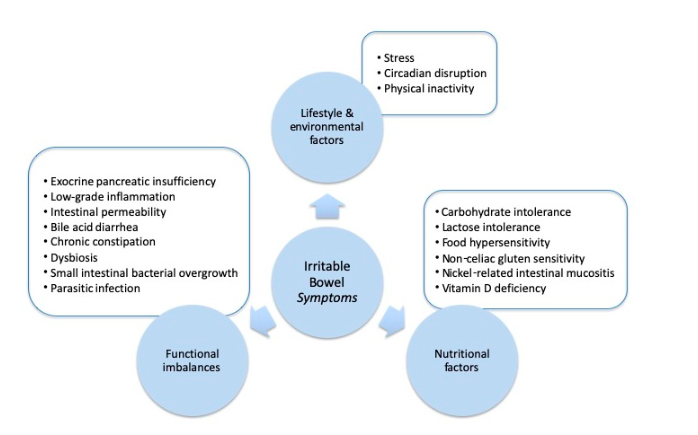
The underlying issues fall into 3 categories:
- Lifestyle & Environment (stress, poor sleep)
- Nutritional Factors (vitamin deficiencies, food sensitivities)
- Functional Imbalances (gut bacteria imbalances, infections)
Within each of these 3 categories, there are a number of aspects that contribute to a disrupted gut. Some examples are listed above but in fact, the research identified 17 factors that have the potential to contribute to IBS.
This may be why medications can be so hit and miss as it can only address one aspect at a time.
IBS (irritable bowel syndrome) after food poisoning
In approximately 10% of those with IBS, it’s reported that symptoms started after a gut infection. This can be in the form of viral gut infections such as norovirus as well as food poisoning. Most commonly this will lead to the diarrhoea form of IBS but it can also lead to constipation.
Studies have indicated that the risk of developing IBS was increased by 4 fold in the 12 months following an infectious event. [Source: Pubmed]
Following infection, there are changes in the gut that will lead to symptoms continuing.
These gut changes include:
- Low-grade inflammation
- Microbiome imbalances
- Intestinal permeability
- Immune changes [Source: NIDDK]
Learn More About Post-Infectious IBS
For some, this can result in changes in the gut that are then diagnosed as SIBO, an overgrowth of bacteria in the small intestine.
Is SIBO the cause of IBS?
SIBO is a condition that has many of the same symptoms as IBS. Several studies have found that an overgrowth of bacteria in the small intestine (SIBO) is present in those with IBS. The number of those with SIBO as the cause of their IBS symptoms may be as high as 78%. [Source: Pubmed]
SIBO is indicated by an increase in bacteria in the small intestine and the symptoms include:
- Abdominal pain or discomfort
- Bloating
- Flatulence
- Changes in bowel patterns [Source: Pubmed]
To cure the symptoms of IBS and SIBO considering the factors that increase the risk of SIBO is important to help address these underlying factors.
The small intestine has several mechanisms that need to be taken place for a well-balanced small intestinal gut microbiome.
These factors are:
- Secretion of gastric juice and bile (these have an antibacterial effect to help balance the small intestine)
- Peristaltic movement prevents the adherence of bacteria into the intestinal mucosa.
- A balanced immune response in the gut.
- The production of beneficial and protective mucus inhibiting pathogenic bacteria.
- Gut antibacterial compounds being produced in the gut.
- A functioning ileocecal valve (prevents the backwards movement of bacteria from the colon to the small intestine. [Source: Pubmed]
These are required to be working optimally for the gut to be healthy. There are also factors outside of the small intestine which can lead or contribute to bacterial overgrowth and the symptoms of IBS (irritable bowel syndrome).
These outside factors include the use of medications and drugs that either alter stomach acid secretions (PPIs), the microbial balance (antibiotics) or small bowel motility (opioids) [Source: NIH]
As SIBO can be the cause of symptoms in many with IBS (irritable bowel syndrome), understanding the factors that have led to SIBO development is important when working to cure IBS symptoms.
High levels of methane can also be seen in the gut which is commonly referred to as IMO (intestinal methane overgrowth). This is highly associated with constipation. [Source: Pubmed]
Treatments & Therapy for IBS (bloating, abdominal pain, diarrhoea, and constipation)
Rather than living on a restricted diet forever, there is another way. By identifying and addressing the underlying issue we can bring about lasting change.
To treat IBS, focusing on the symptoms can be helpful to some extent, but specific approach can be used depending on the underlying condition.
Treatment and support include:
- Short-term elimination diets to assess for food sensitivities
- Strain-specific probiotic supplementation
- Targeted nutritional supplementation
- Testing to assess the gut bacteria
- Supportive lifestyle recommendations
- Gut-directed hypnotherapy
- Cognitive behavioral therapy (CBT)
Food intolerances, diet and IBS
The aim is rarely to find the single dietary culprit that’s linked to the digestive issues. It’s more about supporting and rebalancing it so it’s more resilient and better able to tolerate what we put into it.
However, short term elimination diets can be helpful to take a weight off the digestive system as the underlying issue is addressed.
Best probiotics for IBS
Probiotic supplements can play a wide range of roles in the gut and can be seen as natural medicines. Rather than these bacteria living in the gut forever, they pass through and stimulate the gut in various ways.
This can be to
- strengthen the gut lining
- reduce inflammation
- support digestive processes
- produce anti-microbial compounds
Therefore, it’s important to choose the right strain with the appropriate research behind it.
2 probiotics with most researd for IBS are:
- L Rhamnosus GG
- L Plantarum299V
Other specific strains of bacteria can be used for certain symptoms. For example, Bifidobacterium animalis HN019 has been found to improve bowel movements in those with constipation [Source: Pubmed].
Best supplements for IBS
As well as probiotics a wide range of supplements are available to support the gut. These can be thought of as scaffolding. We erect the scaffolding while we repair. Once the structure is stronger and more resilient we can take the scaffolding down. Along with lifestyle changes, and diet, these can form part of an effective treatment strategy for a condition such as IBS.
These can include gut supplements with research such as:
- Peppermint oil
- L-glutamine
- Prebiotics
- Sodium butyrate
- Vitamin D
Also read: How to Cure IBS Permanetly?
Gut tests for IBS
A range of tests and investigations can be considered to find the underlying issue within the gut. These tests may be via a doctor or specialist.
These gut tests for IBS can provide an include into the gut microbiome as well as the immune response within the digestive tract.
The gut tests for IBS that can be considered include:
- SIBO breath test (assessing for hydrogen and methane)
- Gut microbiome analysis with parasitology (GI 360)
- Food sensitivity testing (IgE or IgA)
- Lactose malabsorption test
- Fructose malabsorption test
- Coeliac disease test
- Faecal calprotectin (to assess for inflammation)
- Pancreatic elastase
Some of these will be recommended via a doctor while of these can order found through The IBS & Gut Health Clinic. The most relevant tests can be selected based on symptoms, health history (e.g., how symptoms started) was well as what tests have been carried out thus far. The aim of these IBS test is to find the underlying cause of IBS symptoms.
Supportive lifestyle recommendations
Lots of stress, exercise and even the times we eat our meals can impact our digestive system and increase the severity of a condition such as IBS (irritable bowel syndrome).
Research indicates that yoga is as effective as a low FODMAP diet. This is a very restrictive diet that removes fermentable fibres, often a trigger for IBS symptoms.
Additionally, gut-directed hypnotherapy is a clinically validated tool that has been found to support the gut-brain connection in those with IBS. As with yoga, this calming practice works to calm the central nervous system and improve the health of the gut.
Irritable bowel syndrome foods to avoid
Even though certain foods can trigger symptoms of IBS, the approach that we like to offer is to not simply understand what food is triggering symptoms but why that food is an issue. If we address the underlying issues in the gut, the gut is stronger and well-balanced and therefore able to tolerate these foods again.
However, in the short term, finding trigger foods can can be a helpful way to manage symptoms and increase the predictability of symptoms and avoid flare-ups.
Common IBS trigger foods include:
- Alcohol
- Caffeine
- Fatty foods
- Spicy foods
- Wheat
- Lactose
To manage symptoms and identify triggers further food restrictions may be considered. A well research approach is the low FODMAP diet which removed highly fermentable (gas producing) foods. These type of fibre may trigger symptoms in those with an underlying imbalance in the gut. These symptoms include; bloating, abdominal pain, constipation and diarrhoea.
A low FODMAP diet may not work for everyone, but several studies have shown improvements in overall IBS symptoms in the range of 68-86% when following this diet. [Source: Pubmed]
Foods that are low in FODMAPs include:
- Protein – beef, lamb, chicken, eggs.
- Certain vegetables – tomato, rocket, celery, aubergine, carrots, potato, courgette
- Certain fruits – berries, kiwi, pomegranates, oranges, pineapple.
- Starches – rice, oats, quinoa
High FODMAP foods include:
- Protein – lentils, beans, chickpeas
- Certain vegetables – garlic, onion, leeks, artichokes, asparagus
- Certain fruits – apples, pears, and cherries
Also Read: Low FODMAP Foods – Everything You Need to Know
Can you cure or treat IBS without medications?
A form of health care for IBS (irritable bowel syndrome) that a doctor may recommend are medications such as mebeverine or buscopan are often recommended for those with IBS. These are medications for IBS that are often needed to be taken on a long-term basis to keep symptoms under control.
The use of supplements, diet and lifestyle suggestions are ways to support the body to bring the gut back into balance naturally.
While some of these strategies to address IBS may also be helpful for long-term gut health and gut health maintenance, they are natural approaches that do not require medication from a doctor.
Can you live a long life with IBS?
Studies have found that in those with IBS symptoms, there is no reduction in life expectancy. This may be counter to the perception of this condition and that the impact on quality of life and well as the impact on mental health does not shorten someone’s life.
One study found that over 50% of those with this condition worry that their IBS will shorten their lifespan. It also found that those with IBS were less likely than those without IBS to die from cancer and had a 19% reduced risk of dying from a psychiatric disease such as anxiety disorder, depression or bipolar disorder. [Source: Pubmed]
Can IBS go away on its own?
It’s common for symptoms of IBS to increase and decrease over a period of time. The period of time when symptoms increase of commonly referred to as flare-ups and for many people with IBS this may last from between several hours to several days.
In these situations, symptoms may go away on their own while in others something is needed to treat the IBS symptoms. This can include changes in diet, supplements and or relaxation practices. [Source: NHS]
Conclusion
So, can IBS (irritable bowel syndrome) be cured? In order to ‘cure’ IBS, we need to see it as a disease. In reality, it needs to be seen as a sign that something is out of balance within the gut. With symptoms such as bloating, abdominal pain and constipation as well as impacts on mental health all potentially being governed by the same underlying issue.
The job at hand is to understand why the symptoms are there and why digestive health has been impacted leading to symptoms of IBS. By supporting the underlying issue we can restore the health of the gut.
Book a free call with us to learn more about our approach and how we can help you.