IBS is one of the most common reasons for a visit to see a GP with the symptoms ranging in severity.
One of the most important processes for anyone with digestive issues is having more sinister causes ruled out. This is where a GP can carry out initial tests or refer on to a gastroenterologist if needed for more in-depth investigations.
These more sinister causes of digestive issues include bowel cancer and inflammatory bowel disease, which for better outcomes need to be caught early.
However, in the absence of these conditions, a diagnosis of IBS is often considered. The ROME IV criteria is a specific set of points that provide clear guidelines for how IBS should be diagnosed. [1]
What are the ROME IV criteria?
The ROME criteria were originally created in the 1990s to assist in the diagnosis of IBS. Since the first version, they have been updated with the most recent version, ROME IV, in 2016.
These were developed by a panel of gastrointestinal experts who have refined the criteria to provide the most accurate guidelines for a clear diagnosis of IBS.
While these criteria were initially intended to guide researchers, they are now also used in clinical practice for GPs and well as gastroenterologists.
Within the ROME criteria, there are also guidelines for how other functional digestive conditions can be diagnosed. For example, if a patient is experiencing loose stools, without the symptoms of pain that is needed for an IBS diagnosis, then functional diarrhoea may be diagnoses, rather than IBS. [2]
The Rome IV criteria for IBS
These criteria state that for a diagnosis of IBS to be given certain factors need to be met. These include:
· Recurrent abdominal pain on average at least 1 day/week in the last 3 months, associated with two or more of the following criteria:
· Related to defecation
· Associated with a change in frequency of stool · Associated with a change in form (appearance) of stool [3]
This set of criteria for IBS is only taking the symptoms the IBS patient is experiencing into consideration. However, further testing may be carried out to rule out gut conditions with similar symptoms of bloating, abdominal pain or altered bowel patterns (e.g constipation or diarrhoea). [4]
NICE guidelines within the UK also offer further symptoms that may be considered when diagnosing IBS. These are not officially within the ROME IV criteria for IBS.
These gut symptoms include:
· a change in the passing of stools – eg, needing to strain, feeling a sense of ‘urgency’ or feeling that the bowels haven’t fully emptied
· bloating, tension or hardness in the abdomen
· a feeling that IBS symptoms are worse after eating · the passing of mucus from the rectum [5]
Different subtypes of IBS
[Image Credit: Health Partners]
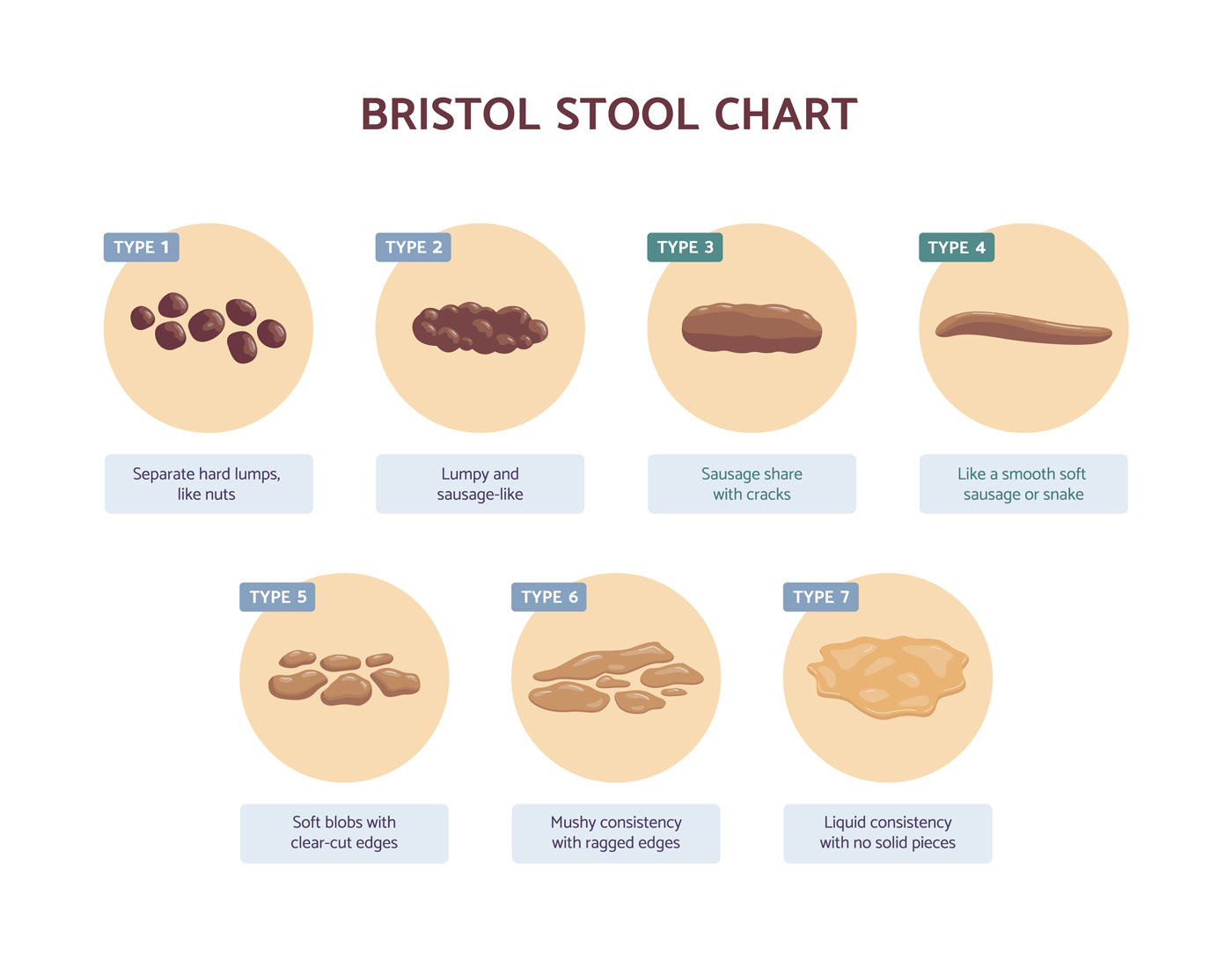
There are 4 different subtypes of IBS which can be made. This type of subtype given to the patient refers to the predominant types of bowel movements they are experiencing.
The 4 types of IBS include: · IBS-D (IBS with diarrhoea)
· IBS-C (IBS with constipation)
· IBS-M (IBS with mixed symptoms of constipation and diarrhoea)
· IBS-U (IBS but their bowel habits cannot be accurately categorized as IBS-D, IBS-C, or IBS-M)
These can be defined as follows:
The IBS-D Subtype
· More than 25% of bowel movements using the Bristol Stool Chart are type 6 or 7
· Less than 25% of bowel movements are type 1 or 2.
The IBS-C Subtype
· More than 25% of bowel movements are type 1 or 2 using the Bristol Stool Chart.
· Less than 25% are type 6 or 7.
The IBS-M Subtype
· More than 25% of bowel movements using the Bristol Stool Chart are types 1 and 2.
· More than 25% are types 6 and 7.
The IBS-U Subtype
· Patients who have the IBS-U subtype meet the diagnostic requirement for IBS, but their bowel habits cannot be accurately categorized as IBS-D, IBS-C, or IBS-M. [6]
How the Rome Criteria Are Used in Diagnosis
The process of using the ROME in clinical practice is the first stage of diagnosis. These are used to assess for abdominal pain, bloating and a change in bowel pattern.
Alongside this, red flag symptoms are also assessed which are to consider more sinister causes of bowel issues. These are symptoms such as unexplained weight loss and blood in the stool.
The NICE guidelines in the UK suggest that the passage of mucus and symptoms being made worse by eating also considered to be factors of note when diagnosis IBS. However they do not need to be present in all cases.
The confirmation of symptoms via the ROME criteria can then lead to further tests to exclude any other causes of symptoms.
These tests include:
· full blood count
· erythrocyte sedimentation rate (ESR) or plasma viscosity
· c-reactive protein (CRP)
· antibody testing for coeliac disease
Further tests are sometimes considered however NICE guidelines state these are not required for an IBS diagnosis.
· ultrasound
· rigid or flexible sigmoidoscopy
· colonoscopy; barium enema
· thyroid function test
· faecal ova and parasite test
· faecal occult blood · hydrogen breath test [7]
Benefits and Limitations of the Rome Criteria
The advantage of the ROME criteria for IBS is that they provide a clear set of guidelines for GPs as well as gastroenterologists. The fact that these criteria have been refined over a number of years by experts in gut health provides support for their use.
These criteria, especially when used in conjunction with the NICE guidelines, also support a patient through considerations for the most appropriate tests. This is to ensure no other conditions are missed during the diagnostic process.
The limitation of the ROME criteria is that they often leave a patient with a diagnosis of IBS with no path forward. This is due to IBS being classified as a functional digestive issue without their being a know cause.
The downside of this is that a patient is often then instructed to self-manage symptoms by avoiding foods, rather than taking into consideration other factors such as dysbiosis, SIBO or low-grade inflammation. [8]
Comparing the Rome Criteria with Other Diagnostic Tools
Another set of criteria for IBS is the Manning Criteria. This was considered more accurate for the diagnosis of IBS than previous versions of the ROME criteria. However, subsequent updates of the ROME criteria now show that it’s more accurate and reliable than the Manning criteria.
However, the Manning Criteria for IBS are very similar with 3 of the following criteria being needed for a diagnosis:
· Pain that starts when bowel movements are more frequent
· Pain that is associated with looser stools
· Pain that is relieved by a bowel movement
· Bloating in the abdomen
· A feeling of incomplete evacuation more than 25% of the time
· Diarrhoea with mucus more than 25% of the time
While blood tests can be helpful in the diagnostic process, it’s often when blood tests are negative that a diagnosis of IBS is more likely. This is due to IBS only being present in the absence of other conditions. [9]
What to Do If You Suspect You Have IBS
If you’re experiencing the symptoms in the ROMVE criteria, a first step can be to visit a GP to have initial tests carried out. This can provide an initial level of clarity into any other factors that may or may not be causing or contributing to symptoms.
This can provide clarity and peace of mind around the symptoms to allow you to move forward with more confidence.
Ahead of these appointments, it may be helpful to keep and food any symptoms diary as well as a list of any factors that may have contributed to symptoms starting. These can be factors such as antibiotics, stress or food poisoning.
Following a diagnosis of IBS it can also be wise to consult with a IBS specialist who will be able to give more in-depth advice and treatment, as well as consider further tests.
Conclusion
The ROME criteria can help to define and provide guidelines for a clear diagnosis of IBS. Perhaps the most important part of this is the exclusion of other more sinister causes, such as bowel cancer.
In the event of an IBS diagnosis, it’s important to remember that even though nothing has been found on tests thus far, this doesn’t mean nothing can be done to resolve symptoms.
This is where working with and IBS and Gut Health Specialist can be the best next step in the process.
FAQs
How to Cure IBS
IBS describes certain symptoms such as bloating, abdominal pain and alterations in bowel patterns. However, the diagnosis of IBS does not indicate what the underlying issue or root cause of these symptoms is.
To resolve the symptoms of IBS, the underlying issue should be examined and addressed.
The underlying cause of IBS does vary from patient to patient, but common causes include the following:
· Food sensitivities
· Gut microbiome imbalances
· SIBO
· Pancreatic insufficiency
· Low-grade inflammation
· Gut-brain axis dysfunction
· Carbohydrate intolerances
· Stress
· Circadian disruption
· Vitamin D deficiency
· Non-celiac gluten sensitivity
To address and resolve the symptoms seen in IBS, the underlying cause should be addressed.
Read More: Can IBS Be Cured?
How long does it take for probiotics to work for IBS?
Probiotics have been shown to provide benefits in IBS patients to improve gut symptoms. Various types of probiotic bacterial supplements have been studied in those with IBS.
While some probiotics may provide improvements in overall symptoms, others have more specific benefits such as improving bloating, flatulence or abdominal pain.
With this in mind, using the right type of probiotic bacterial supplement for specific symptoms is a crucial part of the selection process.
Probiotics rarely provide an immediate benefit and will need to be taken for a period of time before assessing how much benefit they’ve provided. Most studies into the use of probiotics are over a time frame of between 4-8 weeks. In some cases, studies last as long as 6 months. [Source: Pubmed]
How long does it take for peppermint oil to work for IBS?
Peppermint oil has been found to be helpful for the symptoms of IBS. The main compound in peppermint oil is L-menthol which has an antispasmodic effect on the muscles in the gut.
Peppermint oil also has other properties which can help in IBS in other ways. This is due to the peppermint oil also working in a way that is:
· Antimicrobial
· Anti-inflammatory
· Antioxidant
· Anaesthetic All of which can be relevant in the treatment of IBS. [Source: Pubmed]
While studies into the use of peppermint oil for IBS can vary in length, many are within the 4-week time frame. Some of these do however note that an improvement in symptoms is seen in as little as 24-hour hours. [Source: Pubmed]
Can IBS be Cured?
Along with IBS supplements and diets for IBS, a central part of the process of resolving these symptoms is dependent on the underlying issue. This root cause of IBS can vary from person to person.
References
- Aziz I, Törnblom H, Palsson OS, Whitehead WE, Simrén M. How the Change in IBS Criteria From Rome III to Rome IV Impacts on Clinical Characteristics and Key Pathophysiological Factors. Am J Gastroenterol. 2018 Jul;113(7):1017-1025. doi: 10.1038/s41395-018-0074-z. Epub 2018 Jun 8. PMID: 29880963.
- Lacy BE, Patel NK. Rome Criteria and a Diagnostic Approach to Irritable Bowel Syndrome. J Clin Med. 2017 Oct 26;6(11):99. doi: 10.3390/jcm6110099. PMID: 29072609; PMCID: PMC5704116.
- https://theromefoundation.org/rome-iv/rome-iv-criteria/
- Black CJ, Craig O, Gracie DJ, Ford AC. Comparison of the Rome IV criteria with the Rome III criteria for the diagnosis of irritable bowel syndrome in secondary care. Gut. 2021 Jun;70(6):1110-1116. doi: 10.1136/gutjnl-2020-322519. Epub 2020 Sep 24. PMID: 32973070.
- https://www.nice.org.uk/guidance/cg61/ifp/chapter/diagnosing-irritable-bowel-syndrome
- https://www.ajmc.com/view/evidencebased-management-of-irritable-bowel-syndrome-with-diarrhea
- https://www.ajmc.com/view/evidencebased-management-of-irritable-bowel-syndrome-with-diarrhea
- Ghoshal UC, Shukla R, Ghoshal U. Small Intestinal Bacterial Overgrowth and Irritable Bowel Syndrome: A Bridge between Functional Organic Dichotomy. Gut Liver. 2017 Mar 15;11(2):196-208. doi: 10.5009/gnl16126. PMID: 28274108; PMCID: PMC5347643.
- Talley NJ, Phillips SF, Melton LJ, Mulvihill C, Wiltgen C, Zinsmeister AR. Diagnostic value of the Manning criteria in irritable bowel syndrome. Gut. 1990 Jan;31(1):77-81. doi: 10.1136/gut.31.1.77. PMID: 2318433; PMCID: PMC1378344.
History
- Reviewed and updated 9th January 2025 by Martin Cohen