
What is IBS?
Irritable bowel syndrome (IBS) is classed as a functional disorder of the digestive system.
This refers to the fact that while the underlying cause isn’t always fully known, the function of the gut is affected.
It impacts between 7-16% of the western population, with a higher incidence in females than males.
IBS is diagnosed using the ROME IV criteria. This states that for someone to be diagnosed with IBS, they need to be experiencing the following:
Recurrent abdominal pain on average at least 1 day/week in the last 3 months, associated with two or more of the following criteria:
- Related to defecation
- Associated with a change in the frequency of stool
- Associated with a change in the form (appearance) of stool
(These criteria should be fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis.) [Source: Pubmed]
While this can lead to a diagnosis of IBS, the ROME IV criteria does not offer an explanation for why symptoms are happening.
The Causes of IBS
For each person, there is often a combination of factors that lead to IBS.
When addressing symptoms, taking these various aspects into consideration is an important part of the process.
These underlying factors (or root causes) of IBS can fall into 3 main categories.
1. Functional Imbalances
- Exocrine pancreatic insufficiency
- Low-grade inflammation
- Intestinal permeability
- Chronic constipation
- Dysbiosis
- Small intestinal bacterial overgrowth
2. Lifestyle and Environmental Factors
- Stress
- Circadian disruption
- Physical inactivity
3. Nutritional Factors
- Carbohydrate intolerance
- Lactose intolerance
- Food hypersensitivity
- Non-celiac gluten sensitivity
- Nickel-related intestinal mucositis
- Vitamin D deficiency [Source: MDPI]
It can also be the case that more than 1 of these factors contributes to symptoms.
What are the symptoms of IBS?
Central to the symptoms of IBS is pain. This can be cramping in the stomach or intestine.
Pain can also be associated with bloating during IBS flare-ups. This bloating (referred to as distention) can stretch the stomach’s skin and lead to increased sensitivity of the gut lining, referred to as visceral hypersensitivity.
Visceral hypersensitivity is often a key factor when someone does not look distended but feels bloated.
Alterations in bowel movements or the consistency of stool is also a key symptom of IBS. This leads to the subtyping of IBS into 4 main categories.
- IBS-C (IBS with constipation)
- IBS-D (IBS with diarrhoea)
- IBS-C (Mixed IBS)
- IBS-U (Unsubtyped IBS) [Source: Karger]
While symptoms can describe how someone is feeling, they do not explain the underlying reason.
Does food poisoning increase the risk of IBS?
Symptoms of IBS can start slowly over several years. Alternatively, symptoms can appear quickly. One event that can trigger symptoms of IBS is a gastrointestinal infection.
10% of those with an intestinal infection go on to develop long-term symptoms that are consistent with IBS. Depending on the type of pathogen involved, this may increase to 35-45%.
Research estimates that 9% of IBS cases are actually due to a post-infectious situation. [Source: Pubmed]
Post Infectious IBS
Even though many with IBS explain that their symptoms began following a gastrointestinal infection (referred to as post-infectious IBS), it can be hard to estimate true numbers.
This is due to these infections not always leading to a high level of symptoms during the acute phase of the infection. Essentially, the event may not be memorable enough and go unnoticed.
This is the reason why some research indicates this number may be higher.
But when IBS symptoms start following an infection or food poisoning, it is more likely to be of the IBS-D subtype.
Common organisms that may lead to a gastrointestinal infection are:
- Campylobacter
- Shigella
- E. coli
- Salmonella
- Clostridium dificile [Source: Pubmed]
How does IBS develop after food poisoning or an infection?
There are several changes that can occur in the gut that may lead to IBS symptoms.
Three of the observed changes following infection are:
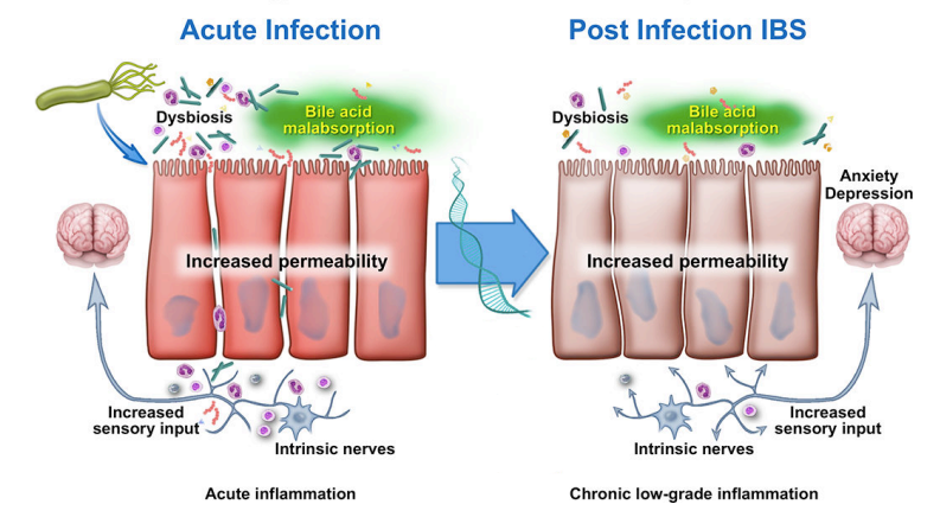
- Low-grade Inflammation
- Endothelial dysfunction/Intestinal Permeability (‘leaky gut’)
- Dysbiosis (bacterial changes)
These types of changes are seen in research where a sample of the small bowel is taken. These microscopic increases in the inflammatory markers are generally termed low-grade inflammation. [Source: Pubmed]
The Gut Microbiome
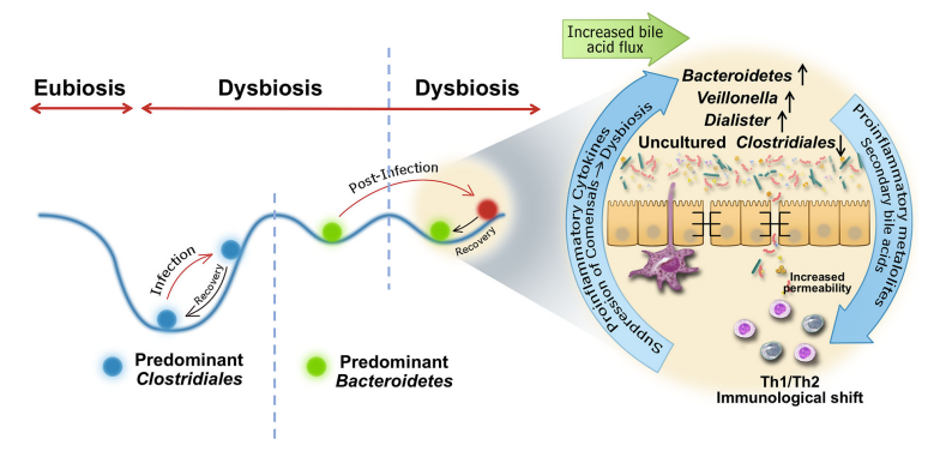
Food poisoning that results in diarrhoea can lead to changes in the bacterial balance in the gut microbiome.
This is likely due to the ongoing inflammatory and immune response in the small bowel.
The immune response (which is inflammatory in nature) is essential to clear the infection. It is understood that the immune system hasn’t entirely calmed down following the infection, which leads to unresolved low-grade inflammation.
These changes in the lining of the digestive tract may then influence the environment in the gut creating a situation that supports the growth of less beneficial organisms.
This imbalance in these bacteria is generally termed dysbiosis. [Source: Pubmed]
It has also been indicated that the balance of the microbiome before an infection influences the risk of post-infectious IBS. Another way to describe this is that if the gut isn’t very resilient, perhaps due to long-term dietary patterns or the use of antibiotics, it may be less able to bounce back post-infection. [Source: Pubmed]
Altered Intestinal Permeability
Altered intestinal permeability is often referred to as leaky gut.
When a small number of PI-IBS patients were assessed with a lactulose/mannitol test (used to assess intestinal permeability), increased intestinal permeability was discovered. However, this appeared to subside and normalise over time.
It may be more noteworthy that the increase in permeability is an early sign of low-grade inflammation. As previously described, this ongoing low-level inflammatory and immune activation may be central to the ongoing nature of post-infectious symptoms. [Source: Pubmed]
These immune changes may also contribute to distention, bloating, and pain. This is due to the increase in specific immune cells (mast cells) and their proximity to nerves, which may trigger these common symptoms of IBS. [Source: Pubmed]
Post Infectious IBS and SIBO
SIBO (small intestinal bacterial overgrowth) is defined as the growth of bacteria in the small bowel in higher numbers than we would typically expect. This is highly associated with IBS, especially the IBS-D subtype. [Source: Pumbed]
When working with IBS, understanding the underlying cause of symptoms is a key part of the process.
The reason for this is that even if there is a positive result on a SIBO breath test, the way that is addressed needs to be modified based on the individual.
As an example, SIBO has been associated with thyroid conditions, abdominal surgery as well as following a gastrointestinal infections, and each of them requires unique considerations.
Even though it may be possible to diagnose SIBO in these individuals, addressing the underlying cause of the bacterial overgrowth needs to be considered. [Source: Pubmed, Pubmed]
As described, in post-infectious situations, this is a combination of immune activation, low levels of inflammation, and alterations along the gut lining that may lead to bacterial overgrowths. [Source: Pumbed]
The Best Diet for Post Infectious IBS.
There is not a single dietary approach that is going to address all of the issues of IBS.
However, a template that can often be helpful to manage symptoms is the low FODMAP diet. This diet limits specific types of carbohydrates found in common foods such as wheat, garlic, onions, beans, and apples.
While these foods are not damaging the gut, if there is an alteration in the absorption or the fermentation of these carbohydrates, symptoms can follow. [Source: Pubmed]
This diet would only be suggested as a short-term approach to help manage symptoms whilst the underlying issue is addressed.
Treatment for Post-Infectious IBS
Several supplements have been indicated to help with addressing the underlying imbalance in post-infectious IBS/IBS after food poisoning.
- Probiotics [Source: Pubmed]
- Prebiotics [Source: Pubmed]
- Herbal antimicrobials [Source: Pubmed]
- L-Glutamine [Source: BMJ]
- Peppermint oil [Source: Pubmed]
Conclusion
With any health condition understanding how and when symptoms began offers an insight into the underlying reason for symptoms.
This allows for a more specific approach to address the mechanisms at the root of the issues.
Finding the right practitioner to support you on this journey is a key part of the process.






