
Intro
IBS attacks or flare-ups can be very unpredictable, often happening unexpectedly.
When symptoms arise, there can be a sense of urgency to calm them and move them back to a more balanced digestive state.
However, it’s not uncommon for the IBS symptoms to be painful and disruptive. This can lead to a state of stress which may only add fuel to the IBS fire. Particularly if we’re unsure what to eat.
In this article, we’ll guide you through the key tools we have to calm an IBS attack.
What is IBS?
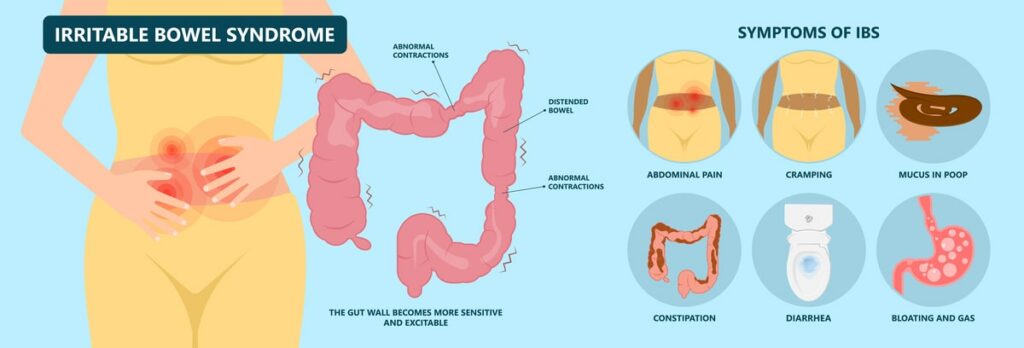
IBS is one of the most commonly diagnosed digestive disorders. Instead of there being a specific test for IBS, IBS is diagnosed based on the presence of certain symptoms.
Symptoms of IBS include abdominal pain or discomfort as well as altered bowel habits (e.g., constipation or diarrhoea). It appears in 10-20% of the global population, but this varies between countries. It’s also twice as common in women as it is in men. [Source: Pubmed]
Along with these symptoms, individuals living with IBS also commonly experience symptoms outside of the digestive system, such as:
Even though there isn’t a specific test for IBS, the symptoms are understood to arise from a combination of several factors.
These include:
- Alterations in motility
- Gut-brain interactions
- Microbiome imbalances
- Bile acid metabolism
- Intestinal permeability
- Mucosal (gut lining) immune activation [Source: Pubmed]
What leads to an IBS attack?
After periods of healthy and balanced gut health, an IBS attack can appear, seemingly from nowhere. It can also be common to have known triggers.
For some with IBS, there are triggers that cause an IBS attack every time. While in others it can be unpredictable. This can make the triggers of an IBS attack harder to pinpoint.
Research indicates that a variety of factors can contribute or increase the risk of an IBS attack. In some cases, a single one of these can trigger IBS symptoms, while for others a combination of a few of these may be what tips the balance.
These include:
- Stress
- Dietary patterns
- Certain foods
- Poor sleep
- Food poisoning
- Alcohol intake [Source: Pubmed]
How long does an IBS attack last?
IBS attacks can last for different amounts of time depending on the individual so once an IBS attack starts it can take time for it to calm down. However, it can be common for the person with IBS to understand how long their attacks last based on previous IBS attacks.
From a research perspective, we also have information on IBS attacks and how long they take to calm down. A study from 2011 reported that an IBS attack can last between 7.9 hours to 36.9 hours.
How often these attacks happen depends on the subtype of IBS someone has. On average, those with IBS-D (the diarrhoea subtype) have 6.3 attacks per month vs. this with IBS-C (the constipation subtype) report 4.4 attacks per month. [Source: Pubmed]
There are things that can be done to calm an IBS attack.
What To Eat During IBS Flare Up
Once an IBS attack starts, calming IBS symptoms (bloating, cramping and bowel changes) as quickly as possible can be a priority.
There are certain foods that may make symptoms worse during flare-ups. These are foods that can:
- Increase gas
- Increase pain
- Increase diarrhoea
- Increasing bloating and flatulence [Source: Pubmed]
The most common culprits include:
- Spicy foods [Source: Pubmed]
- Alcohol [Source: Pubmed]
- High lactose dairy [Source: Pubmed]
- Caffeine [Source: Pubmed]
- High FODMAP foods [Source: Pubmed]
These foods are common triggers yet may not be an issue for everyone experiencing an IBS attack. But in the short term limiting them may be helpful for calming an IBS attack. Once the gut has calmed down these foods may then be reintroduced slowly to ensure they’re ok. It can be that these foods are more problematic during an IBS attack but are ok at other times.
Foods To Avoid With IBS
When symptoms of IBS increase, there can be a change in how our gut responds to food.
It’s not uncommon for a range of foods that were tolerated before symptoms flared to now be an issue. For example, apples and coffee are well tolerated when the gut is happy but for some, during a flare-up these increase IBS symptoms.
It’s also not uncommon for someone to feel as though they’re reacting to everything with even water causing more bloating. This can be where everything that is being eaten or drank causes an increase in symptoms due to the heightened sensitivity in the gut.
A key dietary approach is the low FODMAP diet. This diet limited specific carbohydrates found in many fruits and vegetables. While these foods are healthy, when there are imbalances in the gut, this can lead to sensitivity to high FODMAP foods. This is largely due to alterations in the absorption or fermentation of FODMAPs in the gut of someone with IBS.
A low FODMAP diet may not work for everyone, but several studies have shown improvements in overall IBS symptoms in the range of 68-86% when following this diet. [Source: Pubmed]
Foods that are low in FODMAPs include:
- Protein – beef, lamb, chicken, eggs.
- Certain vegetables – tomato, rocket, celery, aubergine, carrots, potato, courgette
- Certain fruits – berries, kiwi, pomegranates, oranges, pineapple.
- Starches – rice, oats, quinoa
High FODMAP foods include:
- Protein – lentils, beans, chickpeas
- Certain vegetables – garlic, onion, leeks, artichokes, asparagus
- Certain fruits – apples, pears, and cherries
Also Read: Low FODMAP Foods – Everything You Need To Know
It’s also been shown that even a normal amount of gas produced in the gut can be extremely painful. This is often due to increased sensitivity in the nerves along the gut lining. [Source: Pubmed]
The low FODMAP diet essentially takes a strain off a sensitive gut and can be a helpful short-term approach. However, the long-term use of a low FODMAP diet has been indicated to have negative consequences. These include nutritional deficiencies and a negative impact on the gut microbiome. Therefore the Low FODMAP diet is an approach that should be used to manage symptoms rather than something that’s seen as a treatment in and of itself. [Source: Pubmed]
What can I eat with IBS?
During an IBS flare-up, the increase in symptoms can lead to pain and discomfort as well as nausea and fear around food. The combination of these factors can reduce appetite and make understanding what to eat a challenge.
As mentioned, as well as excluding alcohol, caffeine and spicy foods, a low FODMAP diet can help to calm the symptoms of an IBS attack.
The foods to focus on when following a low FODMAP diet include:
Fruits
- Banana (unripe)
- Blueberry
- Cantaloupe melon
- Honeydew melon
- Kiwifruit
- Lemon
- Lime
- Mandarin
- Orange
- Papaya
- Passionfruit
- Pineapple
- Raspberry
- Rhubarb
- Strawberry
Vegetables
- Alfalfa
- Aubergine
- Bamboo shoots
- Bean sprouts
- Bell peppers
- Bok choy
- Carrot
- Cherry tomatoes
- Chicory
- Chives
- Courgette
- Cucumber
- Ginger
- Green beans
- Kale
- Lettuce
- Olives
- Parsnip
- Seaweed, nori Spring onion (green part only)
- Swiss chard
- Tomatoes
Protein
- Meat
- Poultry
- Fish and Seafood
- Eggs
- Bacon
- Firm tofu
- Tempeh
Grains and starches
- 100% spelt bread
- Rice
- Oats
- Polenta
- Arrowroot
- Millet
- Quinoa
- Sorghum
- Tapioca
- Sprouted barley
- White potatoes
- Plantain (green)
- Turnip
- Rutabaga (swede)
- Taro
- Cassava/yuca
- White rice
Drinks
- Water
- Herbal tea (eg – peppermint, rooibos, nettle, berry)
Often using this a shopping list during a flare-up can be the simplest way to approach the diet in the short-term to calm an IBS attack.
How to calm an IBS attack?
Once an IBS attack or IBS flare-up starts, there are additional ways we can work to calm it down.
Diaphragmatic Breathing for IBS
Diaphragmatic breathing is also known as belly breathing and involves activating the diaphragm as we inhale.
This calming breath can support the stress response via the gut-brain axis to move us in the parasympathetic arm of the central nervous system. This is also known as the rest and digestive state. [Source: Bio-Medical]
Herbal teas for IBS
Herbal teas can be a key tool to support and reduce a flare in symptoms. A mixture of caraway, fennel, and anise seeds is often helpful to calm the gut and reduce bloating.
This can be prepared by mixing equal parts of these seeds and then 1 teaspoon. Crushing the seeds and steeping for 20 minutes in 1 cup of hot water and drinking after each meal.
Supplements for IBS flare-ups
Simethicone is an over-the-counter preparation that may support gas balance in the gut. Rather than reducing gas production, this allows gas bubbles to accumulate and join and be passed out of the gut more easily. [Source: Pubmed]
Peppermint oil is another well-researched approach for supporting symptoms of IBS. Peppermint has several modes of action, which include:
- Supporting muscle function in the colon (e.g., antispasmodic)
- Supporting nerve sensitivity
- Anti-microbial (e.g., supporting bacterial balance) [Source: Pubmed]
Digestive enzymes have been widely used to support digestive function and can also be helpful during a flare-up. [Source: Pubmed]
Activated charcoal may also help reduce bloating, but it does also have the potential to lead to constipation and may best be avoided in those will IBS-C. [Source: Pubmed]
Probiotics are a key tool in supporting IBS symptoms. These are part of a strategy to support the underlying imbalances in the gut but may also be helpful in the short term.
Particularly the beneficial yeast Saccharomyces Boulardii which has been indicated to reduce the duration of travellers’ diarrhoea [Source: Pubmed]
Should I Worry About Stomach Gurgling
Stomach gurgling can be a normal part of the digestive process. However, it can be more common in those with IBS. It has been found that high levels of noise and gurgling are found in those with IBS who produce more gas in the gut. While this symptom by itself can be loud or embarrassing it’s not a sign that something more dangerous is happening in the gut.
There are however certain symptoms referred to as ‘red flags’ which would require medical attention
- Abdominal masses
- Rectal masses
- Anaemia
- Rectal bleeding
- Unintentional and unexplained weight loss
- Aged over 60 years change in bowel habit lasting >6 weeks
What Foods Can Cause Stomach Noises
When there are digestive issues certain foods can trigger symptoms of bloating and pain but also increase the noises that come from the stomach. Common culprits include foods containing a high amount of
- Lactose
- Fats
- Spices
- FODMAPs
Eating too quickly and not chewing food adequately can also increase digestive symptoms and the noises from the stomach.
Conclusion
While there are several ways to support your gut during a flare-up and reduce both the severity and duration of these episodes, this is only half of the picture.
We also want to address the underlying issue do these events do not happen at all.






