
Introduction
Irritable bowel syndrome (IBS) is a chronic, yet common condition that causes a range of digestive symptoms. These IBS symptoms can impact approximately 10% of the population and involve symptoms such as cramps, abdominal pain, bloating and gas as well as alterations in bowel patterns. [Source: PubMed]
For many, these symptoms can be mild and infrequent while for others, symptoms can often be severe enough to interfere with daily activities and reduce quality of life.
While dietary changes, exercise and stress management have all been found to improve symptoms of IBS, in this article, we will look at what may cause IBCS with constipation, the options to address these issues as well as symptom management strategies. [Source: PubMed]
What is IBS-C?
Irritable bowel syndrome with constipation (IBS-C) is a type of irritable bowel syndrome (IBS). IBS is a common condition that affects the digestive tract and causes symptoms such as abdominal pain, bloating and changes in bowel habits.
The exact cause of IBS is unknown. However, there are several risk factors that can lead to symptoms. These risk factors can vary from patient to patient. It’s also possible for a combination of these factors to contribute to IBS.
The factors that increase the risk of developing IBS include:
- Alteration in the balance of the gut microbiome
- Low-grade inflammation
- Food intolerances
- Age
- Sex
- SIBO
- Lactose intolerance
- Stress and/or anxiety [Source: MDPI]
For many of those with IBS, their bowel patterns are affected leading to alterations in both the consistency of bowel movements as well as how often they need to visit the toilet.
While the pain and discomfort of IBS can be present in all of those with this condition, it’s possible to refer to a subtype of IBS based on bowel movements. It’s therefore possible to refer to someone as having:
- IBS-C (IBS with constipation)
- IBS-D (IBS with diarrhoea)
- IBS-M (IBS with bowel movements alternating between constipation and diarrhoea)
Research has indicated that 46% of those with IBS and the diarrhoea subtype, while 32% have the constipation subtype. The remaining percentage of IBS sufferers have the mixed subtype. [Source: PubMed]
When assessing for IBS-C, it’s regarding when greater than 25% of bowel movements are of type 1 or type 2 on the Bristol Stool Chart. This is a chart that illustrates the form of the stool, to allow easy description of the stool.
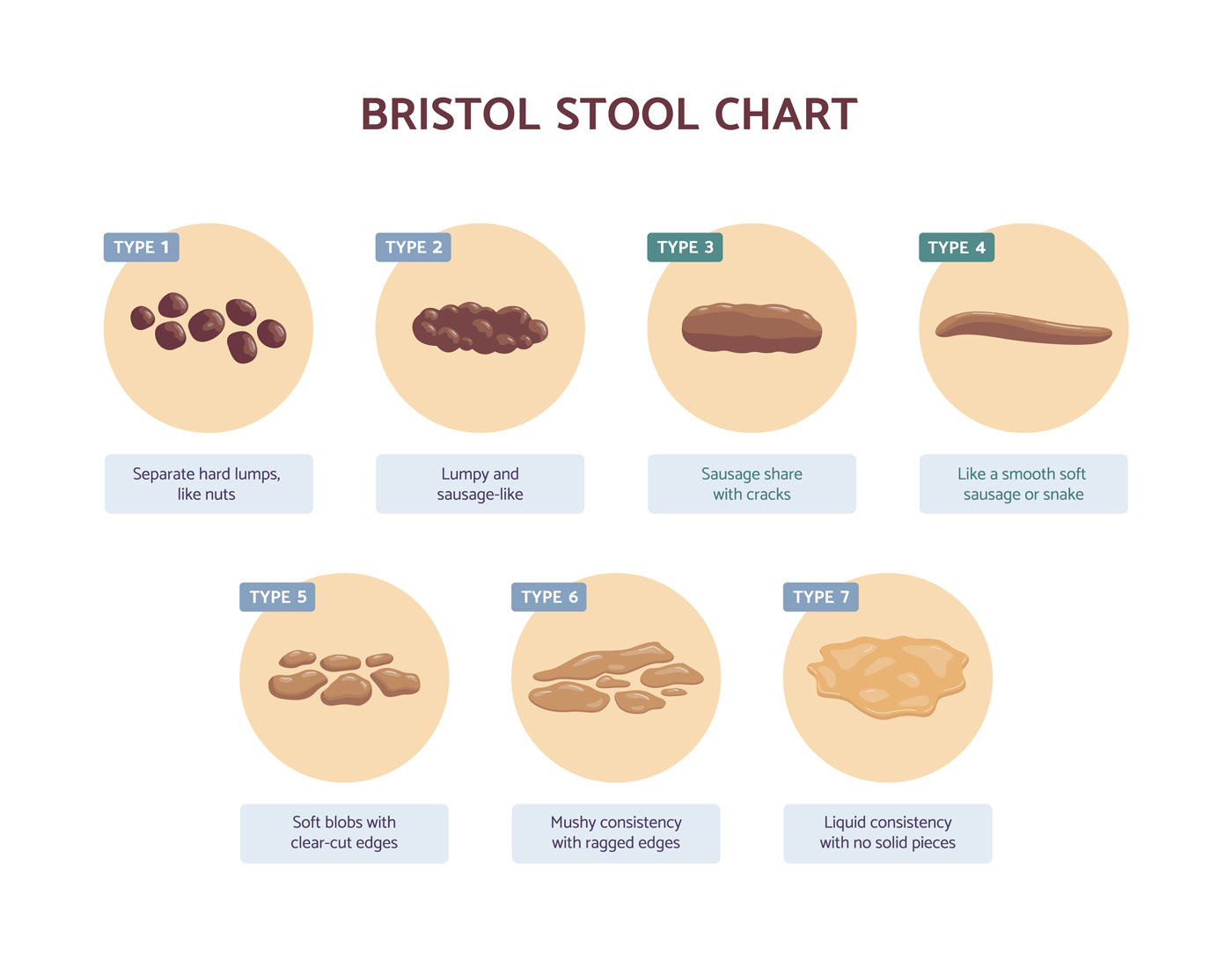
The full range of these stool types are:
- Type 1: Separate hard lumps, like nuts (hard to pass)
- Type 2: Sausage-shaped, but lumpy
- Type 3: Like a sausage but with cracks on its surface
- Type 4: Like a sausage or snake, smooth and soft
- Type 5: Soft blobs with clear-cut edges (passed easily)
- Type 6: Fluffy pieces with ragged edges, a mushy stool
- Type 7: Watery, no solid pieces, entirely liquid [Source: PubMed]
IBS-C Symptoms
For a diagnosis of IBS with constipation, certain symptoms need to be present. These symptoms include abdominal pain or discomfort that improves following a bowel movement.
In addition to this, as already mentioned more than 25% of bowel movements need to be in a certain form to be described as IBS-C.
There may also be additional pain due to constipation. While commonly this can be across the abdomen, it’s also possible for this to be down the left-hand side of the abdomen in the region of the sigmoid colon. Due to this section of the bowel being towards the end of the digestive tract, this area may be under the most pressure for faecal loading. [Source: PubMed]
Although they are not required for a diagnosis of IBS, nausea and vomiting are also 2 symptoms that can appear with IBS. This can be due to which can be caused by gas in the intestines that builds up pressure on nerves in the stomach or intestine walls and causes nausea or an immune response within the gut. This can vary between patients and may be closely related to what is called “dyspepsia” or indigestion. [Source: PubMed]
What is the best natural treatment for IBS-C?
In working to address the treat the cause of IBS-C, there are often 2 elements or considerations to a therapeutic approach. One aspect of the approach is to help improve symptoms via short-term symptom management approaches. The second is to address the cause of the symptoms.
For some individuals, they may have a low dietary intake of certain types of fibres. This may be due to the fact that they’re following a low FODMAP diet, or their diet doesn’t include a wide range of plant foods, such as a Western diet.
In both cases, introducing an additional fibre source may help support digestive function and bowel transit.
- Psyllium Husk is a form of soluble fibre. This means that it dissolves in water and forms the texture of a gel. This type of gel introduces moisture to the bowel and helps with bowel movements. Introducing psyllium husk into the diet has been found to help with bowel movements in those with constipation. [Source: PubMed]
- Flaxseeds also contain a form of soluble fibre that can help with bowel movements in a similar way to psyllium husks. A study from 2020 found that 50g per day of ground flaxseeds significantly improved bowel movements. [Source: PubMed]
When increasing soluble fibre, adequate water intake is also a key element to the success of this approach.
2 of the short-term approaches to improve the symptoms of constipation include:
- Magnesium oxide is a natural stimulant laxative. This works by increasing the water content of the stool which then stimulates a bowel movement. The dose required often varies between individuals but can range between 250mg – 2g per day. [Source: PubMed]
- Ginger has been studied alongside artichoke to support bowel movements and improve symptoms of constipation. The combination of these 2 ingredients was found to significantly improve gastric emptying. [Source: PubMed]
Prune juice has also been well studied and found to improve symptoms of constipation. Importantly, this improves bowel movements but does not lead to overstimulation of the bowels or diarrhoea. [Source: PubMed]
Alongside these approaches, additional considerations can be made to help address the underlying issue within the gut.
What are the best natural supplements for IBS-C?
Probiotics are beneficial bacteria that when taken in the appropriate amount, lead to health benefits. [Source: PubMed]
However, all probiotics do not offer the same benefits. For example, certain strains of bacteria may be more helpful for bloating while others may be more targeted to support constipation.
While several strains have been studied, one that we found most helpful in the clinic for addressing constipation is B. lactis HN019. This probiotic was shown to improve bowel transit time which reduced symptoms of constipation.
This particular strain also has a high tolerance to the acidic environment of the stomach and small intestine. This means that it is well able to survive these conditions. [Source: PubMed]
In addition to probiotics, prebiotics have also been studied and shown to improve gut health and transit time. In particular, the prebiotic PHGG (partially hydrolysed guar gum) has been found to improve many IBS symptoms including constipation.
While this may in part be due to the presence of the fibre which supports motility and movement of stool through the bowel, this prebiotic also supports the growth of key gut species which help with bowel movements and appropriate muscle contractions. Studies found that the inclusion of this fibre resulted in improved bowel movements and a reduced requirement for laxatives. [Source: PubMed]
Primarily, PHGG also supports the growth of Bifidobacteria and Lactobacilli species of gut bacteria. As a result, this is understood to improve the overall ecosystem of the gut, leading to better gut health, and reducing symptoms such as pain and bloating, both present with IBS symptoms. [Source: PubMed]
Are Kiwis good for constipation?
Kiwis have been studied for their benefit in supporting bowel movements and frequency. In clinical studies they have been found to:
- increase defecation frequency.
- increase stool volume.
- improve the softness of bowel motion.
- help to ease defecation.
A large amount of this benefit comes from the dietary fibre within kiwis which is approximately 2-3 grams per 100 grams of fruit.
Further benefit comes from kiwi containing an enzyme called Actinidine which stimulates bowel motility. [Source: PubMed]
Are prunes good for constipation?
Prunes have been studied and found to support bowel movements. They contain a higher amount of fibre than kiwis (6g of fibre / 100g of fruit) but also fructose and sorbitol.
They also contain chlorogenic acids which can help to support the production of digestive enzymes to support the digestive process. In addition to this, these acids may also have a gentle laxative effect leading to less constipation. [Source: PubMed]
Are bananas good for constipation?
Bananas can help with constipation, but this can depend on how ripe the banana is.
Unripe bananas contain a high amount of resistant starch which may in fact worsen or even cause constipation in certain individuals.
However, as bananas ripen, the amount of resistant starch decreases while soluble sugars increase. These ripe bananas contain 3g of fibre / 120g, while this can increase the soluble fibre content, resistant starches are also still present, albeit at a lower level. With this in mind, there are likely better options for fruits to help with constipation. [Source: PubMed]
What is the first-line treatment for IBS-C?
Alongside ensuring adequate water intake, the first line of consideration for IBS-C is fibre supplements like psyllium husk as well as flax seeds.
If these initial approaches do not lead to improved symptoms, further approaches can also be considered.
These include approaches such as:
- Dietary adjustments and adequate fluid intake [Source: PubMed]
- Probiotic supplements [Source: PubMed]
- Prebiotic supplements [Source: PubMed]
- Herbal antimicrobials [Source: PubMed]
- Gut-directed hypnotherapy [Source: PubMed]
What should I avoid with IBS-C?
The balance of the diet can be an important consideration when addressing IBS-C. It can be the case for many that a lower-fibre diet does not provide enough bulk for the stool, thus leading to slower motility.
The reason for this is that processing that is involved in refined products removes a high amount of fibre from this food. The result of this is that most of the food is absorbed in the small intestine, with little fibre remaining in the large intestine.
This means that in the initial stages of treatment for IBS-C, a central consideration may be to remove and avoid processed foods and work to increase dietary fibre.
These processed foods include:
- White breads
- White pasta
- Baked goods (cakes, muffins, doughnuts)
- Sweets and chocolates
- Processed breakfast cereals [Source: PubMed]
By avoiding or limiting these foods, working towards a higher fibre diet can be helpful. However, this transition may need to be slower as many people with IBS symptoms such as bloating or distention can find that an increase in fibre worsens these symptoms.
Therefore, in the short term, a low FODMAP diet may be an important tool to increase certain types of fibres that do not increase bloating. This should be considered a short-term approach to both support bowel movements as well as manage symptoms.
However, the ultimate goal of addressing IBS-C would be for all these higher-fibre foods to be reintroduced without symptoms reappearing. This is where understanding and addressing the underlying issue or reason why the symptoms and food reactions are present is central. [Source: PubMed]
Read more >>> Low FODMAP Foods: Everything You Need To Know
Best Tests for IBS-C
A range of tests are available to assess the possible causes of IBS-C.
SIBO breath tests assess for 2 types of gas, hydrogen and methane. While elevated levels of hydrogen as associated with the diarrhoea subtype of IBS, methane is associated with constipation.
Elevated levels of methane may contribute to constipation via the way in which methane impacts the contractions of the muscles within the gut. The results of this test may therefore guide the approach taken with therapeutic supplements. [Source: PubMed]
Read more >>> Methane SIBO & Constipation Guide
Elimination diets – while there are tests available to assess for food intolerances, the gold standard for assessing food reactions in an elimination/reintroduction diet. This is a process where specific foods are removed for a period of time (commonly 2-4 weeks).
If symptoms have improved, these foods are then gradually reintroduced while symptoms are monitored. It’s common for the foods to contribute to an immune reaction in the gut that builds up over several days, meaning that these can be hard to identify from a food diary alone. Therefore the elimination for a set period of time can provide clarity.
Common foods that contribute to an immune reaction are:
- Milk
- Wheat
- Soy
- Egg
- Corn [Source: PubMed]
Stool tests may help determine whether you have an infection in the digestive tract and identify any bacteria that might be contributing to IBS-C symptoms. While in most cases, infections in the digestive tract lead to diarrhoea, this can still be an appropriate test to understand the balance of the gut microbiome. [Source: PubMed]
Abdominal x-ray/abdominal ultrasound (also known as an abdominal CT scan). While an X-ray uses radiation beams to create images of internal organs and structures; an ultrasound uses sound waves produced by high-frequency electrical impulses.
However, this type of test will often find an impacted stool in the colon (if constipation is present) but it won’t provide the reason why unless there is a structural issue/obstruction in the bowel. [Source: PubMed]
What is the best medicine for IBS-C?
There are 2 main ways that IBS with constipation can be approached.
The first is symptom management. This can be an important strategy to reduce the severity of symptoms to provide short-term relief, however, this may not address the underlying issue.
The second way that IBS with constipation can be approached is to address the underlying issue. This is where addressing the cause of constipation will mean that the symptom management tools are no longer required.
Many of the most common symptom management medications for IBS-C include the following:
- Laxatives are medications that help the body pass stool. They can be used to treat constipation, but they should not be taken for long periods of time or in large doses because they may cause dehydration electrolyte imbalances or in some cases, nerve damage. These options include lactulose and sodium picosulphate. [Source: PubMed]
- Prokinetics are medications that support the appropriate contraction of the muscles in the lining of the digestive tract. These contractions help to regulate bowel movements. This includes medications such as Prucalopride. [Source: PubMed]
- Antispasmodics are designed specifically for people who experience muscle cramps during bowel movements; they work by reducing spasms in the intestines, which may mean there’s less trouble passing stools through the digestive system. [Source: PubMed]
- SSRI antidepressants can help reduce symptoms of depression as well as anxiety related specifically towards bowel movements (such as fear/panic attacks). They have also been indicated to support bowel movements and improve constipation. [Source: PubMed]
Best laxative for IBS with constipation
Laxatives are the only medication that can help relieve constipation. However, it’s important to choose a laxative that won’t cause side effects or make symptoms of bloating or pain worse.
There are many different kinds of laxatives available over-the-counter (OTC) and by prescription.
Some examples include:
- Lactulose
- Sodium picosulfate
- Movicol
- Laxido [Source: PubMed]
Laxatives generally come in two forms: bulk-forming and osmotic. Bulk-forming laxatives work by absorbing water into the stool, softening it so it’s easier to pass through the intestines smoothly. Osmotic agents draw water into the intestine by osmosis (the natural process of passing liquid through a membrane).
This helps soften stools and increase their frequency by encouraging faster transit time through the colon.
It’s important that the dosing guidelines are followed when taking laxatives. Especially when understanding information about taking multiple doses within 24 hours or if there are any other restrictions on when it can be taken (such as avoiding certain foods). [Source: PubMed]
Conclusion
While IBS-C is not a life-threatening condition, it does have a significant impact on someone’s quality of life. This can lead to chronic pain and discomfort as well as fear around eating trigger foods.
While there are many approaches that may lead to improved bowel movements in the short term, it’s important to continue to work to address the underlying factors.
Working with a registered Nutritional Therapist can guide this treatment process.






