
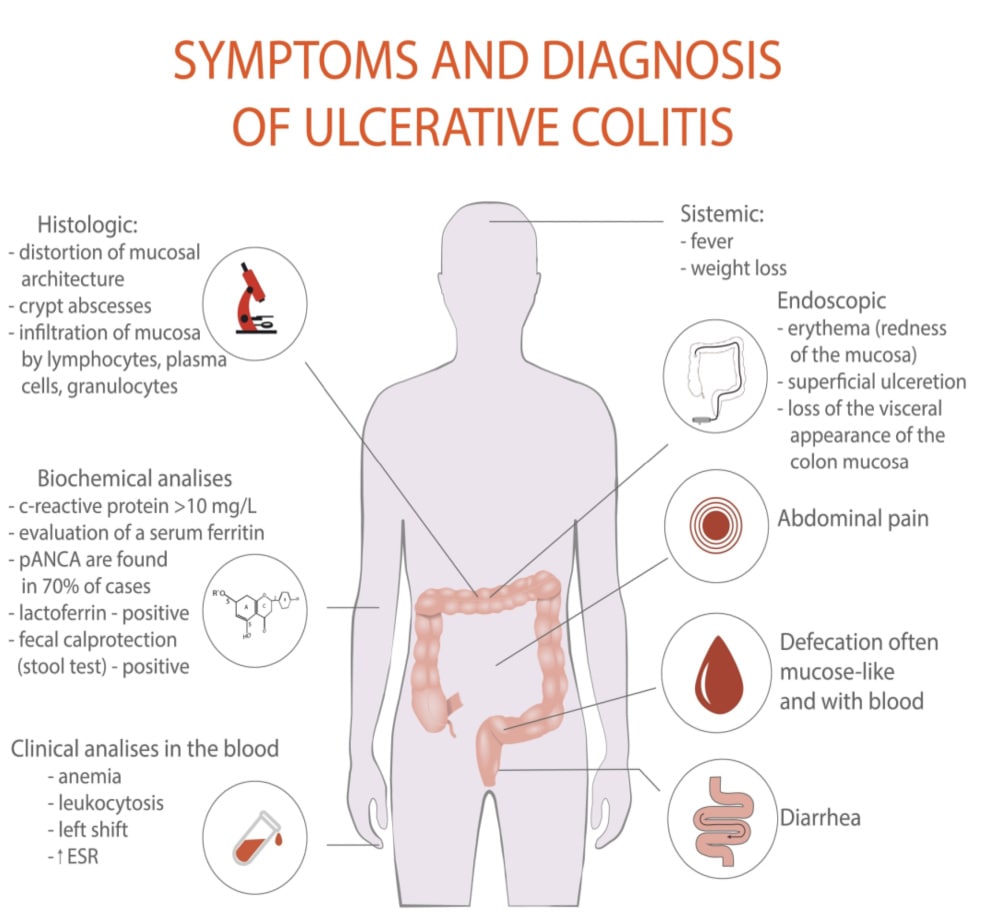
Ulcerative colitis is a form of inflammatory bowel disease that leads to a range of symptoms that include changes in bowel patterns, abdominal pain, and blood in the stool.
Blood in the stool with Ulcerative colitis can be one of the common symptoms of this gut condition and also one of the most worrying. There are some key signs that indicate when there is too much blood.
Ulcerative colitis can impact the gut of individuals of almost any age but the most common range is between 30-40 years old.
The symptoms of Ulcerative colitis present in a way that is characterised by relapses and remissions. This is where symptoms improve or resolve for a period of time, described as remissions. This can be followed by flare-ups in the symptoms of Ulcerative colitis, referred to as relapses. [Source: Pubmed]
The underlying causes of Ulcerative colitis are understood to be due to a combination of factors. These include:
- Genetic predisposition
- Impact on the gut lining
- Imbalances in the immune response
- Environmental factors (for example, bacterial imbalances or food reactions). [Source: Pubmed]
What are the first signs of ulcerative colitis?
Ulcerative colitis can be a long-term digestive disease, however, there may be certain signs of it starting.
The inflammation in the colon may be in different sections which may be different between patients.
At the time of onset:
- 40% present with proctitis
- 30% present with left-sided colitis
- 30% present with pancolitis
The symptoms that can appear first can also vary between patients. In general, they start mildly and increase, with some to severe cases requiring hospitalisation.
The symptoms can include:
- Diarrhoea
- Abdominal pain
- Urgency
- Tenesmus
- Haematochezia (the passage of fresh blood in the stool)
- Blood and mucus in the stool [Source: PubMed]
What is the fastest way to calm Ulcerative colitis symptoms?
During a flare-up of ulcerative colitis symptoms, certain medications may be prescribed to calm symptoms down. This can involve Aminosalicylate medications such as:
- Sulfasalazine
- Mesalamine
Depending on the site of the inflammation in the colon, these medications may given orally as pills or capsules or if the inflammation is towards the rectum a suppository or enema may be prescribed. [Source: PubMed]
It’s also possible to adjust the intake of fibre to calm symptoms down through the use of a low-residue diet. This reduces the intake of certain types of fibre while encouraging the intake of lower-fibre foods.
The aim of this approach is to reduce the intake of the fibres that remain in the bowel, potentially irritating or placing pressure on the bowel. [Source: PubMed]
How much bleeding is normal with Ulcerative colitis?
The amount of blood in the stool of those with Ulcerative colitis can vary. This depends on the main factor of how much of the large intestine (also known as the colon) is impacted but also the level of inflammation in the bowel.
In pancolitis, where the entire large intestine is inflamed, blood in the stool, particularly bloody diarrhoea, is likely to be more prominent when compared to when only a smaller section of the gut is impacted by the inflammation. [Source: Pubmed]
It’s also possible that blood tests will start to show low levels of iron which is termed anaemia. This can also be seen in over 50% of those with Ulcerative Colitis who are currently in clinical remission. [Source: Pubmed].
Symptoms of low iron in Ulcerative colitis
Blood loss is common in Ulcerative colitis. Due to blood containing lots of iron, chronic blood loss in the stool can lead to low levels of iron.
Iron levels can be tested in the blood to monitor levels which may then lead to iron being prescribed in the form of supplements or via an iron infusion. [Source: Pubmed]
Low levels of iron are associated with fatigue which is considered to be a symptom of Ulcerative colitis. Other symptoms of low iron levels include:
- Pale skin
- Reduced exercise capacity
- Shortness of breath
- Tachycardia (a fast heartbeat) [Source: Pubmed]
Iron deficiency anaemia is a common complication of inflammatory bowel diseases (IBD) such as Ulcerative colitis and may be helpful to understand the severity of blood loss. Having regular blood checks can be important to assess iron levels. [Source: Pubmed]
While working to bring the disease into remission is the central approach, restoring iron levels can be helpful to improve quality of life. [Source: Healthline]
Also Read: What Is Pancolitis? Symptoms, Causes & Treatment
Do you bleed a lot with Ulcerative colitis?
Blood in the stool is reported in the majority of those with Ulcerative colitis, while only one-third of those with Crohn’s disease (another form of IBD) report bleeding.
The amount of blood that appears in the stool can vary depending on the disease state. This can range from small amounts of blood that appear on the surface of the stool to higher amounts of blood that turn the toilet water red. [Source: Pubmed]
Can you lose too much blood from Ulcerative colitis?
It is possible to lose too much blood in Ulcerative colitis. While the amount of blood can increase and decrease depending on the disease state, during a flare the amount can increase further.
If you have Ulcerative colitis you can notice a sudden increase in the amount of blood in the stool. This alone may not be a concern, however, if other symptoms also appear and the blood in the stool becomes heavy and continuous this may require more urgent medical attention.
These other symptoms include:
- Infrequent or low urination
- Pale, cold, or clammy skin
- Nausea
- Lightheadedness or dizziness upon standing
- Blurry vision
- Severe abdominal cramping
- Heavy and continuous rectal bleeding [Source: My Crohns and Colitis Team]
A less common complication of Ulcerative colitis is a haemorrhage in the gut. This is where the inflammation in the large intestine reaches a point where a blood vessel ruptures leading to high amounts of blood appearing in the toilet. This is more common in Crohn’s disease than in Ulcerative colitis. [Source: Pubmed]
Ulcerative colitis and when to go to the hospital
Changes in certain symptoms are often described as red flags. These are the symptoms that if they appear or increase in severity may require more urgent medical attention.
These include pale, cold or clammy skin, nausea, blurry vision, severe abdominal cramping, heavy and continuous rectal bleeding as well as infrequent of low urination. [Source: My Crohns and Colitis Team]
How to stop Ulcerative colitis bleeding?
There are many ways that the blood in the stool in Ulcerative colitis can stop. For some, this may calm down by itself. While other interventions may be needed. In severe cases, this may require surgery which may involve the removal of part or all of the colon. [Source: Pubmed]
There are also natural ways to address the underlying factors involves in Ulcerative colitis that leads to bleeding.
Are Ulcerative colitis symptoms worse during period?
Studies have found that those with inflammatory bowel diseases such as ulcerative colitis experience more digestive symptoms, prior to their period. This refers to the same symptoms taking place, however, in those with Ulcerative colitis, they were more frequent.
It has also been found that those with Ulcerative colitis have experienced a higher number of loose stools as well as more abdominal pain during their menstrual cycle.
This means that phase of the menstrual cycle may need to be taken into consideration during the evaluation of Ulcerative colitis. However, according to this study, the symptoms that did not change during the different menstrual phases were:
- nocturnal diarrhoea
- haematochezia (blood in the stool)
- faecal incontinence
- the need for antidiarrheal medications (such as Imodium) [Source: PubMed]
What to eat in an Ulcerative colitis flare
While certain foods can be very well tolerated during good periods of the disease, these may then become an issue during an Ulcerative colitis flare-up.
Once the gut lining becomes inflamed and irritated this can lead to anything passing along it feeling very painful. This irritation along the gut lining not only leads to abdominal pain but can also lead to more blood loss. Removing certain foods for a period of time may help to reduce the strain on the gut and lower levels of the blood being lost.
Ways to reduce the fibres that can irritate the gut include:
- Removing stems and skins from fruits and vegetables
- Cooking and pureeing fruits and vegetables
- Avoiding nuts and seeds
Dairy has also been indicated to be an issue for many people with Ulcerative colitis and can potentially contribute to a flare. If a specific food is leading to an immune reaction may then contribute to the inflammatory response which damages the gut and causes blood loss in the stool of those with Ulcerative colitis.
Removing dairy may calm the immune response and flare-up. A 2014 study concluded that the intake of dairy products may increase the severity of Ulcerative colitis. [Source: Pubmed]
Is Aloe vera good for Ulcerative colitis?
Aloe vera has been shown to help reduce inflammation and improve gastric ulcers. This also has antioxidant properties which support the health of the gut lining and reduces the damage to the tissue in the gut. [Source: Pubmed]
However, aloe vera is also used as a natural laxative and therefore may need to be approached slowly in some patients with Ulcerative colitis.
Are probiotics good for Ulcerative colitis?
While there is a range of probiotics on the market, not all have been researched for inflammatory bowel diseases such as Ulcerative colitis. This means that probiotics need to be selected carefully for Ulcerative colitis.
A specific probiotic, called VSL#3, has been researched in Ulcerative colitis which lead to a remission/response rate of 77%. This study also reported zero negative reactions (side effects) to taking this probiotic for Ulcerative colitis. [Source: Pubmed]
What is the best type of turmeric to help with Ulcerative colitis?
Turmeric is a herb that is used in a range of cooking practices and traditional medicines. The active component of this herb is called curcumin.
This concentrated form of curcumin has been studied to help reduce inflammation. One study using this form of turmeric alongside the medication mesalamine noted a 300% improvement in response when compared to a placebo. [Source: Pubmed]
Conclusion
There are several ways to calm down a flare-up that has led to more blood appearing in the stool. This can be helpful to calm down symptoms in the short term.
The long-term approach that can be provided by The IBS & Gut Health Clinic is to help to reach a state of remission and to reduce the risk of another flare-up happening in the future.






