What is Endometriosis?
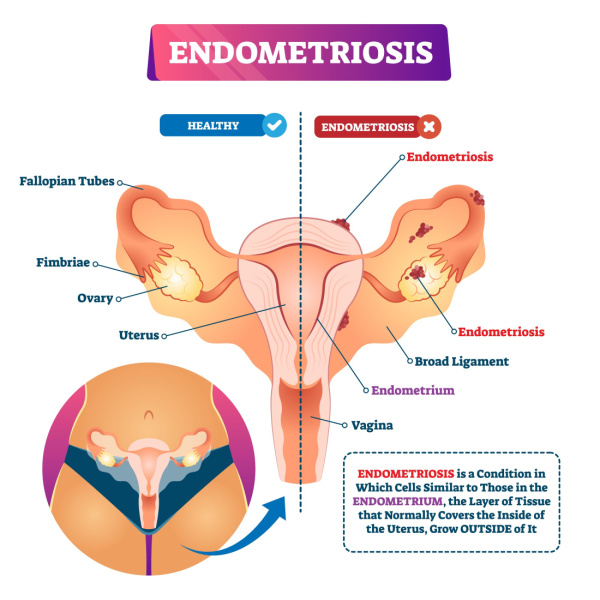
Endometriosis is a chronic gynaecological condition which is understood to impact 10-15% of women of reproductive age.
Endometriosis can lead to a range of symptoms. The symptoms of endometriosis include:
- dysmenorrhea (pain associated with menstruation)
- chronic pelvic pain
- dyspareunia (painful intercourse)
- infertility [Source: PubMed]
In endometriosis, there is the growth of the endometrial lining outside of its normal location, the uterine cavity. In endometriosis, this ectopic endometrium is most commonly located in the ovaries, but it can also be found in areas such as:
- pelvic peritoneum
- uterosacral ligaments
- fallopian tubes
- broad ligaments [Source: PubMed]
What Causes Endometriosis?
While a single cause of endometriosis development isn’t known there are several theories. These theories of endometriosis development include the retrograde flow of menstrual fluids, alterations in the immune system and increased inflammation.
An aspect of the theory that involves the retrograde flow of menstrual fluids can also include, the translocation of the microbiome.
Certain imbalances in this microbiome may they lead to changes in the immune response and increase inflammation. [Source: PubMed]
Other theories include the increased presence of endocrine-disrupting chemicals (EDCs) in the environment. This is due to their link or possible ability to interfere with hormonal actions. These compounds include heavy metals and pollutants. [Source: PubMed]
Also Read: Endometriosis and IBS – What’s the Connection?
Dysbiosis and Endometriosis
Dysbiosis refers to imbalances in the microorganisms that inhabit the body. These organisms include bacteria, viruses and fungi and regulate functions in the body that include the immune system, digestive health and mental well-being.
Whereas the term microbiome refers to all of the microorganisms that live on the external or internal surfaces of the body, specific regions can be defined. For example, the gut microbiome refers specifically to all of the microorganisms within the digestive tract. Whereas the reproductive tract microbiome refers to the organisms in regions such as the vagina and the uterus. [Source: PubMed]
Imbalances in these organisms occur in ways that include an increase in potentially pathogenic (or harmful) microbes, or a reduction in the levels of health-promoting microbes.
Dysbiosis has been associated with many conditions that include:
- IBS
- IBD
- Cancer
- Arthritis
- Psoriasis
- Endometriosis [Source: PubMed]
Not only does the gut microbiome regulate inflammatory processes, but it can also influence estrogen metabolism. This imbalance in the gut microbiome not only impacts gut health but can contribute to or influence hormonal conditions such as endometriosis.
Furthermore, reductions in beneficial or protective organisms such as Lactobacilli, make the microbiomes (both in the gut and the female reproductive tract) more susceptible to less beneficial organisms. [Source: PubMed]
In the female reproductive tract microbiome, if Lactobacilli organisms were reduced or depleted, this was associated with poor reproductive health. This is in part explained by the ability of these organisms not only to lower the pH of the microbiome but also producing compounds called short-chain fatty acids. Both of these aspects aid in prohibiting the growth of harmful microbes.
Additionally, dysbiosis and reductions in these bacteria is also understood to contribute to an inflammatory response in the endometrium. [Source: PubMed]
Also Read: How is Endometriosis Diagnosed?
Endometriosis, the Microbiome and Gut Health
Whereas the microbiome refers to the entire microbial population in the human body, each location has its own microbiome. This is where the terms gut microbiome or vaginal microbiome can be used.
Studies have examined the composition of various microbiomes in those with endometriosis. For example, a 2019 study compared the vaginal, cervical and gut microbiome. In the cervical microbiome, a higher abundance of potentially pathogenic organisms was found. These organisms included; Gardnerella, Streptococcus, Escherichia, Shigella and Ureaplasma. While in the gut microbiome Shigella and Escherichia, 2 potentially pathogenic bacteria, were dominant.
This study highlighted the common element of dysbiosis is various microbiomes in endometriosis. [Source: PubMed]
The link between endometriosis and gut health may be due to inflammation. This can be due to the action of inflammation in the peritoneal area contributing to the production of inflammatory chemicals (cytokines). These chemicals can travel to the digestive tract and play a role in altering gut function. This can be due to their ability to suppress gastric acid (stomach acid) and alter gut motility.
These changes then alter the intestinal environment, making it less hospitable to beneficial organisms, and allowing for the over-growth of potentially pathogenic organisms. This link between the role of the inflammation seen in endometriosis and how this impacts gut function, leading to gut dysbiosis. [Source: PubMed]
Dysbiosis and Bacterial Vaginosis
Dysbiosis is commonly seen in digestive conditions such s IBS as well as hormonal diseases such as endometriosis. A similar situation of dysbiosis is also reported in bacterial vaginosis.
In bacterial vaginosis, the depletion of protective bacteria such as Lactobacillus and the simultaneous overgrowth of pathogenic microbes are observed.
These pathogenic organisms include:
- Gardnerella
- Prevotella
- Bacteroides
The organisms are also associated with other hormonal/gynaecological conditions such as:
- Endometriosis
- PID
- Infertility
- Endometritis [Source: PubMed]
Is IBS common if you have endometriosis?
IBS and endometriosis are commonly found in the same patients. In fact, studies have reported a 5 times higher rate of IBS in women with endometriosis when compared to women without endometriosis.
As described already, there are several possible reasons for this link between IBS and endometriosis. These include:
- Endometrial inflammation can impact bowel function
- Mucosal inflammation leading to dysbiosis
- Visceral hypersensitivity
- Endometrial adhesions [Source: PubMed]
In addition to the inflammatory and or microbiome changes, there is also a phenomenon referred to as the “cross-organ” effects. This theory is based on the changes to the central nervous system due to nerve signalling from the endometriotic tissue which can then impact gut function. This theory supports the fact that endometriosis can impact digestive health and gut function, even without bowel-involved endometriosis.
The Best Diet for Endometriosis
With the high occurrences of digestive symptoms in those with endometriosis, dietary approaches can be considered to improve symptoms.
One common diet that is used to manage symptoms is the Low FODMAP diet. This was found to improve symptoms in those with IBS-type symptoms, for example, symptoms of bloating, pain and altered bowel patterns. This study concluded that those with IBS and endometriosis were more likely to see an improvement in their symptoms when compared to those with IBS alone. [Source: PubMed]
Alongside the low FODMAP diet, a range of other diets has been considered to help those with endometriosis. At the core of these are natural and whole-food diets that focus on a diverse range of plant foods and high-quality protein. These also consider restricting certain foods that may aggravate the gut, the immune system of inflammatory processes.
These diets include:
- Mediterranean diet
- Gluten-free diet
- Low nickel diet
- Elimination diet
How to Treat Endometriosis and Dysbiosis
Before targeting the microbiome directly, it’s important to set a firm foundation for health. This includes factors such as sleep, stress management as well as daily movement/exercise.
These lifestyle factors may contribute to the ongoing nature of symptoms and also increase their presence. For example, high levels of stress can alter the microbiome leading to dysbiosis. It can also increase pain perception. Therefore, stress management practices such as deep breathing, yoga and mindfulness meditation have been found to improve quality of life and reduce pain in those with endometriosis. [Source: PubMed]
In a similar way, exercises and daily movement have been shown to improve several symptoms of endometriosis. This has been linked to the improvement in mental health due to exercise as well as the anti-inflammatory and gut-regulating benefits of physical activity. [Source: PubMed]
Additionally, acupuncture has also been shown to improve outcomes in endometriosis. A recent study found that a 5-week course of weekly acupuncture treatment lead to improvements that included:
- A decrease in pelvic pain
- A decrease in pain during intercourse
- Improved quality of life
The benefits of acupuncture were noted 2 months after the end of the course of treatment. [Source: PubMed]
Are Supplements Helpful for Endometriosis?
A range of supplements has been studied in relation to endometriosis and appear to act via different means. For example, ensuring adequate levels of certain nutrients can reduce the risk of developing endometriosis while others are reported to reduce lesion size, reduce pain or reduce inflammation.
- Vitamin D
- Zinc
- Magnesium
- Omega 3
- Curcumin
- Quercetin
- N-acetylcysteine
- Probiotics
- Resveratrol
- Alpha Lipoic Acid
- Vitamin C
- Vitamin E
- Selenium
- Epigallocatechin3-gallate [Source: PubMed]
It is unlikely that all of these supplements need to be taken at the same time to see a benefit. However, a combination of selected supplements can often be more beneficial that taking 1 in isolation.
This is part of the reason why working with a trained professional can help to personalise the approach.