
IBS and endometriosis are 2 separate health conditions. One is primarily a bowel issue that can present in men as well as women. The other is a reproductive issue that only impacts women.
However, there is a distinct link between these 2 conditions.
This article will explore this connection and explain how these conditions can be diagnosed and also addressed.
What is endometriosis and what is IBS
Studies have found a clear link between hormones and digestion. This is indicated by the fact that IBS is twice as common in females as it is in males. While this does not always mean that hormone imbalances are responsible for digestive issues, they can play a role.
Understanding each of these conditions individually can be helpful in understanding the link between them. [1]
Endometriosis
Endometriosis is considered a chronic inflammatory condition where the tissue normal only found lining the uterus is found outside of the uterine cavity.
The most common symptoms of endometriosis are:
· Dysmenorrhea (painful menstruation)
· Menorrhagia (heavy or prolonged menstrual bleeding)
· Chronic pelvic pain
· Gastrointestinal symptoms (e.g. bloating, pain, altered bowel patterns)
Early detection of endometriosis can improve outcomes however, the average time before a diagnosis is made is 5-6 years. During this time, it can also be common for women to receive the diagnosis of IBS.
While features (e.g. low-grade inflammation, increased intestinal permeability and visceral hypersensitivity) are associated with both conditions the management and approach vary between conditions.

IBS
IBS is described as a functional digestive condition. This refers to the altered function of the gut, without an identified cause.
However, there can be a range of underlying factors that can increase both the risk of developing IBS symptoms.
The common symptoms of IBS include:
· Bloating
· Abdominal pain
· Altered bowel movements (constipation or diarrhoea)
It’s also common for IBS patients to experience:
· Headaches
· Food intolerances · Changes in mood (eg: depression or anxiety) [2]
Are IBS and endometriosis linked?
It has also been indicated that IBS and endometriosis are related to chronic stress psychological disorders. In both IBS and endometriosis, the severity of the digestive symptoms correlates with psychological well-being.
The difficulty here is determining whether the altered psychological well-being is something that is causing further issues (e.g. IBS symptoms) or it’s the result of chronic health concerns.
Visceral hypersensitivity (a general increase in pain sensation) has also been seen in both conditions. While this may be originating from the site-specific to the condition, it may also be originating from elsewhere, such as peripheral inflammation. [3]
What are the causes?
Rather than being a single cause of either endometriosis or IBS, there are a range of factors that can increase the risk of developing these conditions.
IBS Risk Factors | Endometriosis Risk Factors |
|
|
What are the symptoms and similarities?
When examining the symptoms of IBS and endometriosis there are key similarities in the symptoms but also distinct differences.
While endometriosis symptoms can often increase and decrease in relation to the menstrual cycle, they can also contribute to ongoing abdominal issues.
Often, a complicating factor is that with abdominal discomfort, it can be a challenge to know whether or not this is stemming from the gut or the reproductive system.
The following chart highlights the symptoms of both of these conditions, including the symptoms shared between the 2.
IBS Symptoms | Endometriosis Symptoms |
|
|
How are they diagnosed?
While there are commonalities between IBS and endometriosis, both in the symptoms and causes, they are diagnosed in different ways.
This can be via blood tests, stool tests and well as scans and internal examinations.
Diagnosing IBS
The lack of a clear test to diagnose IBS results in a firm diagnosis of IBS being left to the criteria used. For example, the ROME IV criteria state:
Recurrent abdominal pain on average at least 1 day/week in the last 3 months, associated with two or more of the following criteria:
1. Related to defecation
2. Associated with a change in the frequency of stool
3. Associated with a change in the form (appearance) of stool
These criteria should be fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis. [5]
This does not, however, offer a clear reason for the symptoms. It can be the case the digestive symptoms associated with endometriosis may mistakenly be diagnosed as IBS.
It has also been noted that the medications used to treat endometriosis may worsen the digestive symptoms. This means that the side effects of these medications may be contributing to the digestive issues reported. [6]
Diagnosing endometriosis
Laparoscopy is considered the gold standard for diagnosing endometriosis. This is however an invasive procedure.
Therefore, pelvic examination and imaging techniques such as transvaginal ultrasound (TVS) and magnetic resonance imaging (MRI) are often considered.
Read More: How Is Endometriosis Diagnosed?
What are the treatment options?
When examining these conditions in isolation, there can be specific approaches that focus on each issue. There will of course be an overlap.
For example, focusing on supporting the microbiome in IBS can help treat endometriosis. Also, helping to reduce the inflammation seen in endometriosis will go a long way to support IBS causes.
The specifics are as follows:
Treatment for IBS
A central aspect of any IBS treatment strategy is to understand the root cause of the symptoms.
For some, their symptoms may be the result of food poisoning and yet for others, it may be the result of an imbalance in hormones or stress levels.
Understanding these factors will lead to an approach that has an increased chance of resolving gut issues for good.
The treatments for IBS include:
· Probiotics
· Prebiotics
· Antimicrobials herbs
· Peppermint oil
· Digestive enzymes
· Antibiotics
· Gut-directed hypnotherapy
Treatment for endometriosis
A range of approaches for addressing endometriosis exist. Some involve pharmaceuticals and surgery while others can be via supporting the gut, supporting hormones and reducing inflammation.
· Laparoscopic surgery – to remove affected endometrial tissue
· Hysterectomy – to remove the uterus
Natural approaches include:
· Dietary – food rich in omega-3 fats and antioxidants
· Gut support – probiotics and prebiotics
· Curcumin – to reduce inflammation
· Fish oil – to reduce inflammation
· Green tea – to support hormone balance
· Wild yam – to support hormone balance · Isoflavone-rich foods – to support hormone balance [7]
When to seek professional advice
Due to the risk of infertility, if endometriosis is suspected it should be something to see a doctor about. The earlier it is diagnosed, the better for long-term outcomes.
If there is pain that increases over time or gets worse during sex of after a bowel movement, medical advice should be sought. This would be investigated and rule out any other conditions.
Additionally, from a digestive perspective, certain symptoms are classed as red flags. These mean that medical advice should be sought and further tests possibly carried out.
These red flag symptoms include:
· Passing blood
· Pain that increases after a bowel movement
· Unexplained weight loss
· Abdominal masses
· Family history of ovarian cancer
· A family history of bowel cancer
Working with a medical practitioner or gut health specialist can help identify and address possible causes of these symptoms.
FAQ’s
Can endometriosis cause IBS-like symptoms?
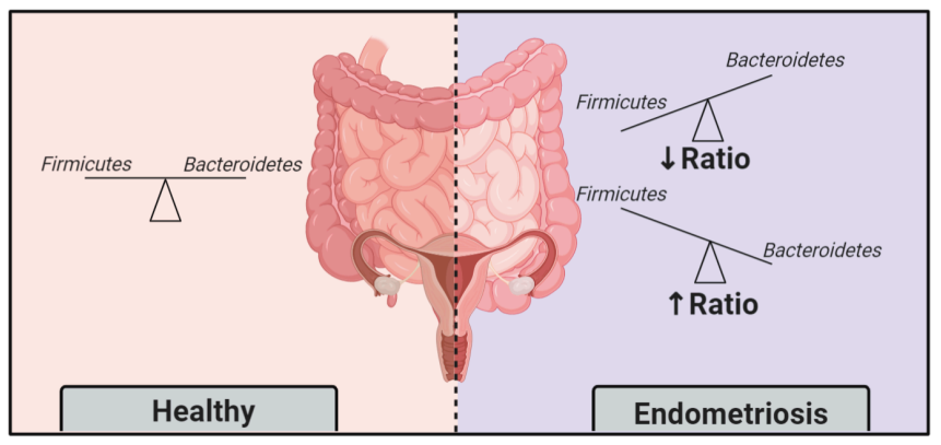
Yes, endometriosis can cause IBS-like symptoms. This can be due to the endometrial growth putting pressure on the bowel, changes in the balance of the gut bacteria as well as inflammation.
Can you have endometriosis and IBS?
It’s possible to have both endometriosis and IBS it is common. Studies have found that 20% of those with endometriosis also have IBS. [8]
Does IBS make endometriosis worse?
It hasn’t been found that IBS makes endometriosis worse, but increased abdominal discomfort from IBS can increase the pain of endometriosis. This increase in pain does not mean that the endometriosis has spread, but it can certainly make the patient feel less comfortable.
It may also provide less clarity as to where the pain is originating.
History
Updated by Martin Cohen – 22nd September 2024
References
Anbardan, Sanam Javid et al. “Gender Role in Irritable Bowel Syndrome: A Comparison of Irritable Bowel Syndrome Module (ROME III) Between Male and Female Patients.” Journal of neurogastroenterology and motility vol. 18,1 (2012): 70-7. doi:10.5056/jnm.2012.18.1.70
Zamani M, Alizadeh-Tabari S, Zamani V. Systematic review with meta-analysis: the prevalence of anxiety and depression in patients with irritable bowel syndrome. Aliment Pharmacol Ther. 2019 Jul;50(2):132-143. doi: 10.1111/apt.15325. Epub 2019 Jun 3. PMID: 31157418.
Davide Viganò, Federica Zara, Paolo Usai, Irritable bowel syndrome and endometriosis: New insights for old diseases, Digestive and Liver Disease. Volume 50, Issue 3, 2018. Pages 213-219. ISSN 1590-8658. https://doi.org/10.1016/j.dld.2017.12.017.
Parasar, Parveen et al. “Endometriosis: Epidemiology, Diagnosis and Clinical Management.” Current obstetrics and gynecology reports vol. 6,1 (2017): 34-41. doi:10.1007/s13669-017-0187-1
Lacy, Brian E, and Nihal K Patel. “Rome Criteria and a Diagnostic Approach to Irritable Bowel Syndrome.” Journal of clinical medicine vol. 6,11 99. 26 Oct. 2017, doi:10.3390/jcm6110099
Saidi K, Sharma S, Ohlsson B. A systematic review and meta-analysis of the associations between endometriosis and irritable bowel syndrome. Eur J Obstet Gynecol Reprod Biol. 2020 Mar;246:99-105. doi: 10.1016/j.ejogrb.2020.01.031. Epub 2020 Jan 25. PMID: 32004880.
Ricci AG, Olivares CN, Bilotas MA, Bastón JI, Singla JJ, Meresman GF, Barañao RI. Natural therapies assessment for the treatment of endometriosis. Hum Reprod. 2013 Jan;28(1):178-88. doi: 10.1093/humrep/des369. Epub 2012 Oct 18. PMID: 23081870.
Salmeri, Noemi et al. “Microbiota in Irritable Bowel Syndrome and Endometriosis: Birds of a Feather Flock Together-A Review.” Microorganisms vol. 11,8 2089. 15 Aug. 2023, doi:10.3390/microorganisms11082089






