
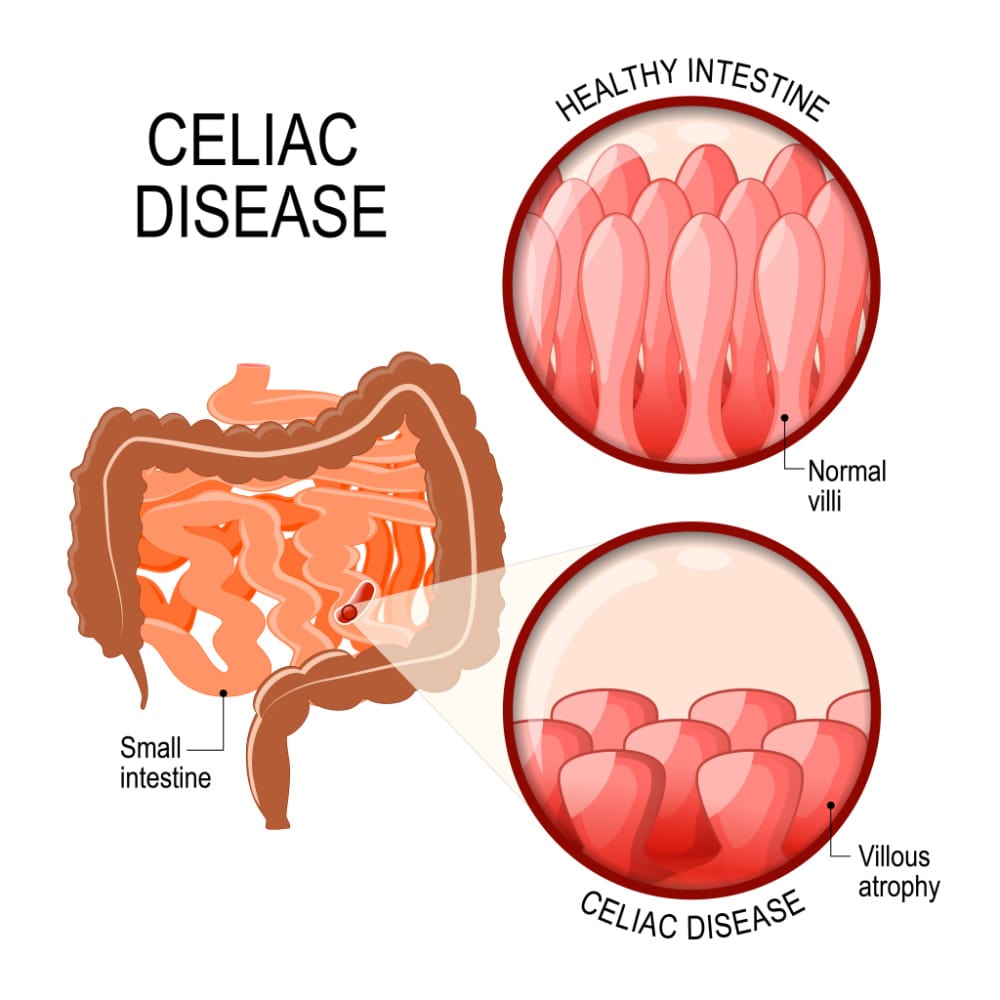
Coeliac disease is classed as an autoimmune condition that originates from an altered immune response to gluten. The autoimmune response to gluten in those with the condition leads to damage to the lining of the digestive tract which then leads to poor absorption of nutrients. This can then lead to many of the symptoms associated with this condition.
The autoimmune response to gluten cannot be reversed. This means that gluten needs to be permanently avoided if you have Coeliac disease. However, if gluten is avoided it is possible for the gut lining to recover and for symptoms to resolve. [Source: Pubmed]
Coeliac disease is one of the most diagnosed genetic conditions. In Europe and the United States, this condition is present in 1-2% of the population. However, is it believed that many cases remain undiagnosed [Source: Pubmed]
Those at a high risk of developing Coeliac disease include:
- Relatives of patients with the condition
- Those with symptoms associated with the disease (diarrhoea, abdominal pain, constipation
- Those with associated disorders (type 1 diabetes, down syndrome, anaemia, infertility, osteoporosis) [Source: Pubmed]
What causes Coeliac disease?
The 2 main factors that increase the chance of coeliac disease are genetics and the environment.
Certain genes are a very high association with coeliac disease. These are described as HLA genes. Over 90% of those with Coeliac disease, express these genes. It is accepted that these genes are the main risk factors in leading to the onset of the condition. However, not all of those with these genes develop Coeliac disease other factors are involved. This includes further genes that increase susceptibility as well as environmental factors. [Source: Pubmed]
Environmental factors are also understood to contribute to the onset of Coeliac disease. These factors include:
- Feeding patterns in the first year of life [Source: Pubmed]
- Viral infections (e.g. rotavirus) [Source: Pubmed]
Breastfeeding has a protective effect on the infant, particularly when related to food allergies. One study found that children being breastfed at the time of gluten introduction had a 52% reduced chance of developing coeliac disease.
The same study also estimated that if all babies in the UK were breastfed at the time of gluten introduction this could lead to 2500 fewer cases of coeliac disease each year. [Source: Pubmed]
Studies have found that certain infections (e.g. viruses such as rotavirus) can increase the risk of coeliac disease autoimmunity. This risk of Coeliac disease increases with the increased number of infections. [Source: Pubmed]
A 2014 study reported that increased levels of mercury are found in the blood and urine of coeliac disease patients following a gluten-free diet. This can potentially be attributed to genes that contribute to an altered response to mercury exposure. [Source: Pubmed]
Also Read: How To Go Gluten Free
Symptoms of Coeliac disease
The symptoms of Coeliac disease can vary depending on the age, how long the disease has been present and also if other gluten-related issues are being experienced outside of the digestive tract.
Coeliac disease was initially believed to appear only in infants, however, in recent years its diagnosis has become more common in adults. [Source: Pubmed]
The most common set of symptoms in Coeliac disease is similar to what may be seen in IBS and SIBO. These generally appear early in life after gluten-containing foods are introduced. [Source: Pubmed]
Also Read: What To Eat With an IBS Attack
The digestive symptoms of Coeliac disease include:
- Diarrhoea
- Malabsorption
- Abdominal pain
- Distension and bloating
- Vomiting
- Weight loss
Coeliac disease can also lead to symptoms outside of the digestive tract. These non-gastrointestinal symptoms can include:
- Dermatitis herpetiformis
- Chronic fatigue
- Joint pain/inflammation
- Iron deficiency anaemia
- Migraines
- Depression
- Attention-deficit disorder
- Epilepsy
- Osteoporosis/osteopenia
- Infertility and/or recurrent fetal loss
- Vitamin deficiencies
- Short stature
- Failure to thrive
- Delayed puberty
- Dental enamel defects
- Autoimmune disorders [Source: Pubmed]
Foods that contain gluten
Gluten can be found in a range of natural and processed foods.
Gluten-containing grains include:
- Wheat
- Varieties wheat (wheatberries, durum, semolina, spelt, farina, farro, graham)
- Rye
- Barley
- Brewer’s Yeast
Common Foods That Contain Gluten include:
- Pasta
- Couscous, and gnocchi)
- Noodles (ramen, udon, soba (those made with only a percentage of buckwheat flour) chow mein, and egg noodles – rice noodles and mung bean noodles are gluten-free)
- Bread and Pastries
- Baked Goods
- Cereal & Granola
- Beer (unless specifically labelled as gluten-free)
- Brewer’s Yeast
There are additional foods that can contain gluten, however, this does depend on the manufacturer and the production.
These can include; energy bars, chips/fries, processed meats, soups, syrups, and soy sauce. [Source: Celiac.org]
Coeliac disease test
The most widely used test to assess for Coeliac disease is a blood test. This test for Coeliac disease measures Anti-tissue transglutaminase antibodies (tTGA). This is carried out via the ELISA methodology (enzyme-linked immunosorbent assay).
Measuring IgA anti-endomysial (IgA EMA) antibodies is a test that can be used to confirm Coeliac disease in those with a positive tTGA. This test has a high level of specificity. However, approximately 2-10% of those with Coeliac disease have an IgA deficiency which can lead to a false negative result. For this reason, total IgA can also be assessed. [Source: Pubmed]
A biopsy (sample) of the small intestine is considered the gold standard (the best) test for diagnosing coeliac disease. This sample is then analysed to assess for changes along the digestive tract which include villous atrophy and decreased enterocyte height. [Source: Pubmed]
Conclusion
The removal of gluten from the diet can lead to a resolution in symptoms. In some, the removal can lead to an improvement with other symptoms still persisting.
This can be due to a variety of factors that include imbalances in the gut bacteria, sensitivities to other foods or IBS.
Working with a Registered Nutritional Therapist can help identify and address these other aspects that may contribute to the ongoing nature of symptoms and help to restore your gut health.






