What is candida in stool?
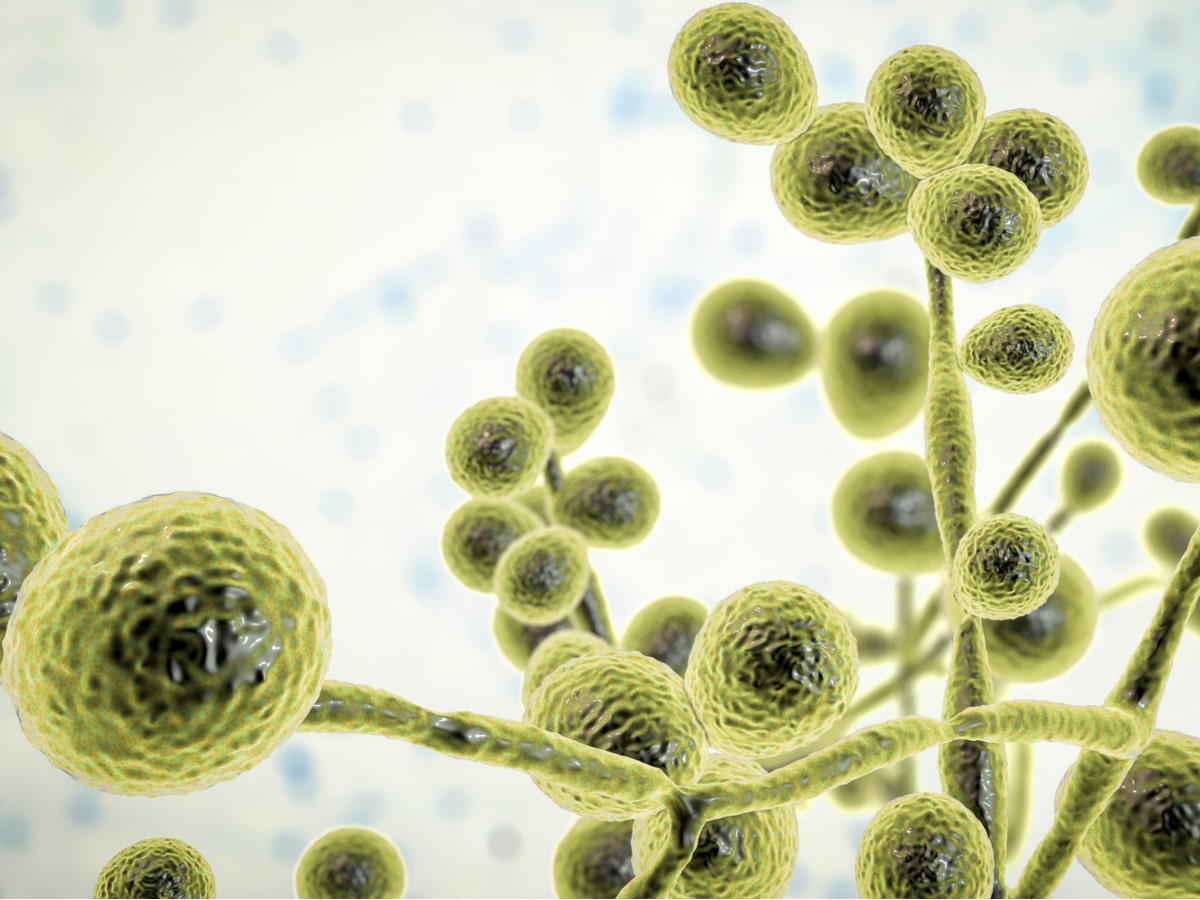
The human body is colonised by thousands of organisms. These include bacteria as well as yeasts such as candida.
Candida is a healthy and normal part of the human gut microbiome. It’s also present in the oral microbiome and urinary microbiome. The candida genus contains over 200 different species, but only a few of these can be potentially problematic by leading to candida infections.
If the microbiome becomes less stable, the balance of these organisms can change and may then lead to a higher number of these organisms than we’d typically like to see.
These overgrowths or imbalances in these microorganisms may then lead to a candida overgrowth and a range of IBS-type symptoms.
These can include: bloating, distention, and changes in bowel patterns. [Source:Pubmed]
This may lead to a change in the gut microbiome and make the environment more hospitable to candida. This is often referred to as a candida infection or intestinal candidiasis.
However, rather than think of candida purely as an infection, it’s more like an opportunistic organism. If the overall environment within the gut microbiome has changed, it becomes less stable, and candida may take advantage of this.
The term used to describe this is pathobiont. Healthy in normal levels but has the potential, given the right environment to cause harm. [Source:NCBI]
What leads to increased levels of candida in stool?
A well-balanced and healthy gut microbiome is a stable and resilient environment. This means it’s able to keep any less beneficial organisms under control.
However, if there are changes in the gut or changes in how the body regulates the gut microbiome, then candida may start to overgrow. This may then result in symptoms of candida in the stool.

Commonly, candida overgrowths can occur when the individual’s immune system is compromised. It can also happen gradually due to long-term dietary patterns or after a course of antibiotics. [Source:Pubmed]
This is because many of these antibiotics promote the growth of fungal species (e.g., candida) due to the disruption of the gut microbiome.
They eliminate key organisms which could have otherwise inhibited the fungal species. [Source:NCBI]
Are there different types of candida overgrowth?
Candida imbalances can be classed as either superficial or invasive.
Superficial infections impact the skin or the mucosal membranes (e.g., the lining of the digestive tract.
Invasive means it may invade the bloodstream and disseminate to internal organs. Risk factors for this include:
- Surgery (especially abdominal surgery)
- Burns
- Long-term stay in an intensive care unit
- Previous administration of broad-spectrum antibiotics
- Immunosuppressive agents [Source:NCBI]
What are the symptoms of candida in the bowel?
While research is mixed, many of the most common symptoms of a candida overgrowth are digestive in nature.
These symptoms of candida include:
- Belching,
- Bloating
- Indigestion
- Nausea
- Diarrhea
- Gas
This was noted in research exploring the possibility of fungal/candida overgrowth in the small intestine. This was termed SIFO (small intestinal fungal overgrowth). This was indicated to be possible in non-immunocompromised individuals. [Source:Pubmed]
Candida can also lead to symptoms outside of the digestive system. These include:
- Brain fog
- Tiredness
- Fatigue
- Joint pain
This may be due to candida metabolites entering the general circulation and impacting another part of the body.
However, this may not be solely due to candida, as when the gut microbiome becomes dysregulated, there can also be imbalances in other organisms.
What are the causes of candida overgrowth?
Adjustments and alterations in the gut microbiome can lead to gradual changes that can influence the levels of candida.
A key indicator of a healthy microbiome is the pH of the colon. An optimal pH has been indicated to be on the slightly acidic side. This slightly acidic environment is primarily driven and influenced by the beneficial fermentation process.
As they’re fed with plant fibres, key species of gut bacteria produce certain acidic compounds that help balance the gut. These acidic compounds also influence the overall environment of the microbiome.
As long as the pH of this environment is maintained, then an organism that is considered optimistic (such as candida) will find the ecosystem less hospitable and be less able to overstep their mark.
This can be seen with adequate support of lactobacillus species which also produce hydrogen peroxide, which inhibits the growth of candida. [Source:Pubmed]
Can antibiotics cause candida?
While antibiotics are like saving in many instances, they can impact the gut microbiome. A key way they can do this is by clearing the way for opportunistic organisms to overgrow.
Antibiotics used in patients, as the name implies, only have action against bacteria. Whereas anti fungal medication will have action against fungal species such as candida.
If antibiotics are used, and the bacteria populations may then be impacted. This disturbance can lead to symptoms of IBS but also allow for fungal such as candida species to repopulate the gut. Because these aren’t impacted by antibiotics, they can almost see this as their opportunity to take charge of the gut ecosystem.
The risk is higher for the use of broad-spectrum antibiotics. [Source: Pubmed]
How is candida addressed?
The approach to addressing candida issues varies from person to person but can include 3 main areas:
- Diet
- Lifestyle support
- Supplements
Diet
Diet is a crucial tool we have to support the balance of the gut microbiome and levels of candida. While certain foods can worsen digestive symptoms, a foundational support is to work to have the diet as varied as possible.
Within this variety including highly fermentable foods such as garlic, onion as well as beans, and pulses can support the pH of the colon. However, these foods are often not very well tolerated in those with symptoms such as bloating and changes in bowel patterns.
To help support these symptoms, a low FODMAP diet may be helpful in the short term. The aim of this diet is to reduce the levels of fermentation taking place to improve symptoms. This diet does not starve the bacteria or candida in order to kill them and should only be used in the short term. [Source:NCBI]
Lifestyle Support
One of the key areas that can influence the balance of the microbiome and the immune system is stress levels.
Stressful events have been indicated to reduce the resilience of the microbiome and the immune system along the gut lining. These changes can allow for opportunist organisms such as candida to take hold.
Stress can also alter our relationship with food and lead to less healthy choices.
Simple breathing practices can be an important foundation support if stress is ongoing.
Additionally, supplement such as ashwagandha, Rhodiola and magnesium may be helpful to support the central nervous system. [Source: Frontiersin]
Supplements
In some cases, when the gut is pushed out of balance, it can realign itself with time. In other instances, it may need a helping hand.
Key tools that can be used include:
Antimicrobial herbs
These are herbs and herbal extracts that have an antifungal activity to support the microbial balance and levels of candida.
These include:
- Garlic
- Oregano
- Cinnamon
- Berberine containing herbs [Source: NCBI]
While these can be helpful, they are not intended for long-term use.
Prebiotics
A key prebiotic that has been shown to influence colonic pH is lactulose and the balance of candida in the stool.
Supporting the appropriate pH balance may improve the overall quality of the ecosystem and make it less hospitable for candida. However, any prebiotic should be started with caution as it may cause a degree of bloating and gas in some. [Source: BMJ]
What are the symptoms of Candida in stool?
Symptoms of candida in the feces or stool can be wide-ranging. This can include digestive symptoms such as bloating and changes in bowel patterns as well as food intolerances.
It can also contribute to symptoms outside of the intestines. This can be in the form of skin issues as well as anxiety.
These symptoms outside of the intestines can be caused by candida overgrowth within the gut. This can be due to the irritation to the gut lining and compounds produced by the candida leading to changes to the gut-brain connection. [Source: PubMed]
What is the cause of Candida in stool?
While candida is not a bad thing as such, higher levels can be an issue. This can lead to health challenges, gut symptoms, food intolerances and in some cases require medical attention.
Candida can be considered an opportunistic organism. This means that if presented with the right opportunity it will overgrowth, potentially leading to health issues.
In a large number of patients, the issue with candida happens when the person’s immune system is not as strong as it could be.
This is where candida infections are often an issue that is secondary to a compromised immune system. Those with a compromised immune system include:
- Those undergoing cancer treatment
- Those taking immune suppressive medication following organ transplantation.
- Genetic immune deficiencies
- Advanced or untreated HIV infections
- Active treatment with steroids [Source: CDC]
These may be considered more serious or extreme cases of immune suppression.
It’s also possible for high levels of candida to be present in the stool following the use of antibiotics. In this instance, one of the most common symptoms is diarrhoea, commonly termed antibiotic-associated diarrhoea.
Due to the impact of antibiotics on the gut microbiome, candida can overgrow to fill the space left in the gut. In many cases, the gut can rebalance itself once the course of antibiotics has been completed. However, in others, imbalances in the levels of these organisms within the gut may persist and require support. [Source: PubMed]
This can often be seen as an infection. However, in many cases, it’s due to an overgrowth of this organism.
How do you get rid of Candida in your stool?
Low-level imbalances or overgrowths of candida in the stool can often respond to approaches such as probiotics, dietary changes and in some cases medications such as fluconazole.
In some patients, the imbalances in the gut may have an underlying factor that needs to be taken into consideration also.
For example. this can be in the form of an inflammatory bowel condition such as Crohn’s disease. Those with this gut issue have been found to have a high level of candida in the stool than healthy controls. [Source: PubMed]
Conclusion
Once the gut microbiome becomes dysregulated, we can see a range of imbalances in the bacteria as well as yeasts like candida.
Targeting the organisms that are overpopulated with antimicrobial herbs can often be a vital part of the protocol.
However, supporting the overall health of the host and the ecosystem is also integral for long-term gut health.






