
Small intestinal bacterial overgrowth (SIBO) occurs when excessive bacteria build up in the small intestine, often due to slowed food and waste transit caused by conditions like surgery or disease. This bacterial overgrowth can lead to symptoms such as diarrhea, bloating, and changes in stool consistency, often resulting in weight loss and nutritional deficiencies. SIBO is diagnosed through breath tests and stool analysis, and treatment typically involves antibiotics and dietary changes.
What is SIBO?
SIBO (small intestinal bacterial overgrowth) is a condition that involves a higher level of bacteria in the small intestine than would typically be seen. This can lead to many of the symptoms seen in IBS, such as bloating, changes in bowel patterns, and abdominal pain or discomfort.
The most accurate way to assess SIBO is to aspirate and culture the fluid from the small intestine. This involves taking a sample of the liquid from the small intestine which is then assessed for the concentration of bacteria. However, this test is not routinely carried out in clinical settings, with a SIBO breath test being the preferred option for assessment.
These bacteria can be similar to those normally seen in the large intestine rather than the small intestine. [Source: PubMed]
What are the symptoms of SIBO?
The symptoms of SIBO are what is typically seen in most patients with IBS. These symptoms include:
- Bloating
- Abdominal pain
- Food intolerances
- Flatulence
- Weakness
- Fatty stools
- Vitamin deficiencies
- Changes in stool form
- Changes in the frequency of bowel movements
For most with SIBO, there is a high level of bacteria in the small intestine that produce hydrogen. This gas is most commonly associated with diarrhoea and urgent bowel movements.
Methane can also be produced in the digestive tract. This can occur either in the small or the large intestine. Even though this is an overgrowth of organisms in the digestive tract, the organisms that produce methane are not bacteria; they are officially classified as archaea. [Source: PubMed]
Until recently, the term ‘methane-SIBO’ has been used, however, since the SIBO does not accurately describe an overgrowth of archaea, the term IMO (intestinal methane overgrowth) has been used more recently to describe an overgrowth of methane-producing organisms. [Source: PubMed]
The overgrowth of methane is more commonly associated with constipation as the main type of bowel movement.
Are there different types of SIBO?
In hydrogen-positive SIBO, the bacteria found in the small intestine can vary with 2 dominant patterns of bacteria. The 2 well-established types are:
- UAT (upper aerodigestive tract) SIBO
- Coliform SIBO
The organisms present in UAT (upper aerodigestive tract) SIBO are predominantly bacteria from the mouth. These include Prevotella sp. and Streptococcus viridans.
The organisms present in coliform SIBO are primarily from the first section of the large intestine. These bacteria include Escherichia coli, Klebsiella pneumoniae, Proteus mirabilis, Enterococcus sp., or Clostridioides sp.
Even though these bacteria and types of microbial balance may differ. The differences between the 2 types may not be clinically relevant as the same approach is likely appropriate for both types. [Source: PubMed]
These 2 types of bacterial balance would likely involve diarrhoea and not constipation.
How do you treat SIBO constipation?
When treating methane-SIBO/IMO, there are generally 2 considerations to the approach.
- Lowering the levels of microbes in the gut
- Working to address the underlying reason
Working to lower the levels of the overgrown bacteria involves considerations such as antimicrobial herbs and antibiotics. It has also been found that using the right strains of probiotic bacteria can also help to normalise gas levels in the gut. [Source: PubMed]
For many with SIBO, there is often an underlying issue or reason for the overgrowth. If this underlying cause is not taken into consideration, then it can often be likely that symptoms return following the antimicrobial treatments.
While there isn’t a single cause of SIBO, some of the causes include:
- Resection of the ileocecal valve
- Small intestinal dysmotility
- Low-grade inflammation
- Low stomach acid
- Coeliac disease
- Crohn’s disease
- Immunodeficiency [Source: PubMed]
What kills SIBO naturally?
Since an overgrowth of methane-procuring organisms is highly associated with constipation, working to address and target the levels of these organisms in the gut is required.
Herbal antimicrobials can be seen as natural antibiotics. These are commonly used to target methane-producing organisms.
These herbs include:
- Garlic (allicin) [Source: Pubmed]
- Neem [Source: Pubmed]
- Clove oil [Source: Pubmed]
- Peppermint oil [Source: Pubmed]
Other compounds can also be helpful to lower levels of methane to improve constipation. One of these is soy isoflavones which help to lower levels of hydrogen, which in turn lower levels of methane in the gut. [Source: PubMed]
The use of tannin-rich herbs has also been studied in cattle to reduce levels of methane production. These include cinnamon and cloves. [Source: PubMed]
Prebiotics have also been found to help with improving constipation as well as reducing methane levels. For example, the prebiotic GOS has been shown to reduce levels of methane. While beneficial in studies, it’s common for prebiotics to be introduced cautiously to reduce the risk of any increase in gas or bloating. This can be common when modifying the microbiome with prebiotics. [Source: PubMed]
Another prebiotic, PHGG has been found to increase the level of beneficial gut microbes Bifidobacterium and lactobacilli, which can improve the microbial ecosystem. It’s also been found to help normalise stool in the of constipation and diarrhoea.
This means this prebiotic can be helpful for a range of digestive symptoms. However, as will the prebiotic GOS, a slow introduction of this prebiotic is often required to reduce the change of side effects. [Source: PubMed]
Which antibiotics are best for SIBO?
Antibiotics have also been studied to address the microbial overgrowth in SIBO and IMO. The most well-studied antibiotic for hydrogen-dominant SIBO is the antibiotic rifaximin. While various doses have been studied, a dose of 1650mg/day of rifaximin for 14 days is considered appropriate.
In cases where methane is overgrown, the antibiotic neomycin is often used alongside rifaximin at a dose of 1000mg per day. [Source: PubMed]
How does SIBO affect bowel movements?
SIBO breath tests measure the levels of 2 gases in the test samples. These are hydrogen gas and methane gas.
While most people with SIBO and symptoms of IBS will experience bloating, gas, and abdominal discomfort, it’s common for people to experience diarrhoea or constipation.
For the most part, those with hydrogen-dominant SIBO will experience diarrhoea. This is often due to the malabsorption of sugars or the malfermentation of fibres, leading to increased gas or an influx of liquid into the bowel. This will then trigger a bowel movement.
On the other hand, methane SIBO can lead to slow bowel movements. This is commonly due to how methane inhibits the action of certain muscles in the bowel wall. This reduces the muscle’s ability to contract, leading to slow motility. [Source: PubMed]
What does SIBO stool look like?
The type of stool that may be seen in SIBO depends on whether someone is constipated or is experiencing diarrhoea.
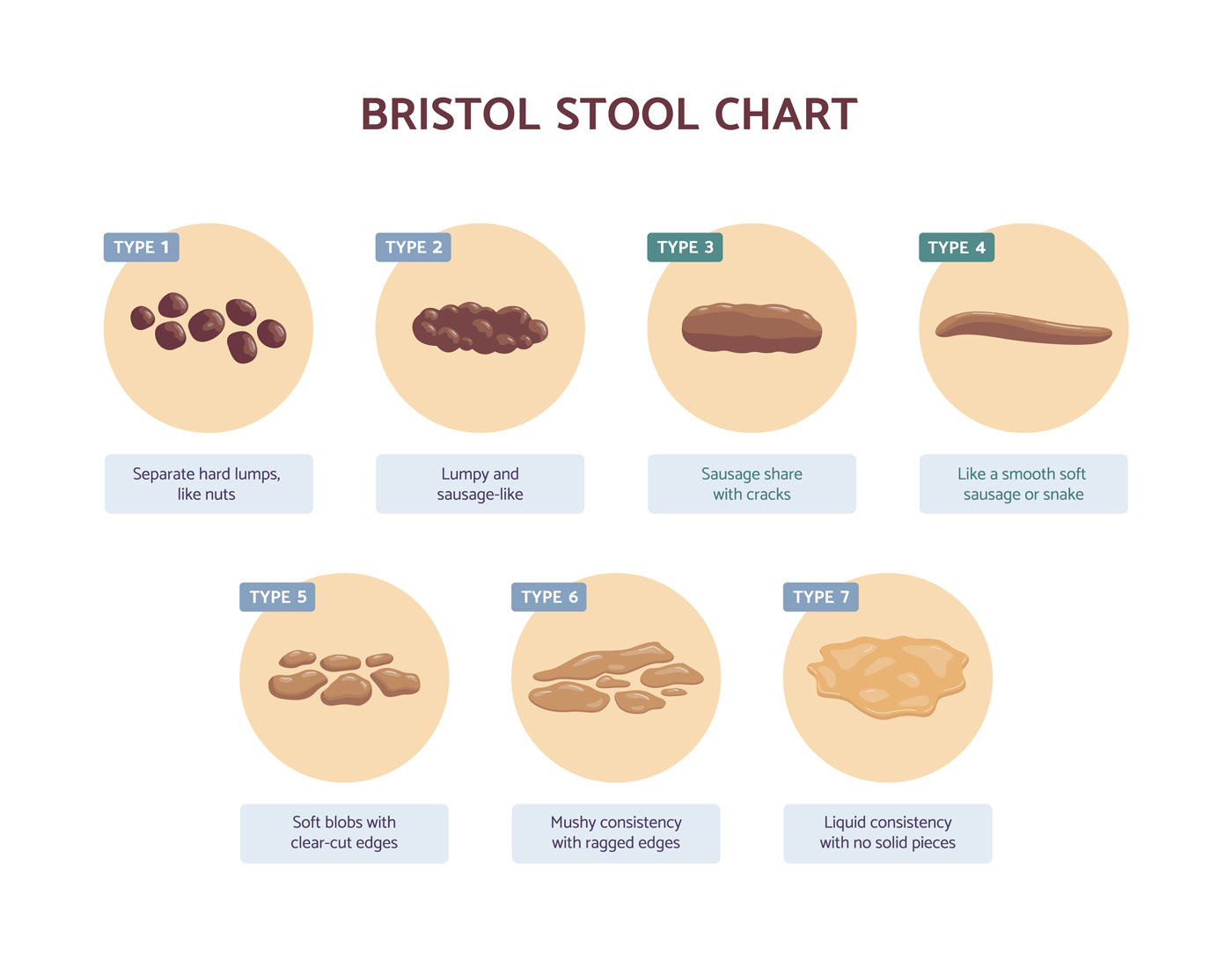
When describing the form of stool isn’t helpful to use the Bristol Stool Chart, with constipation being between 1 and 2 on the stool chart and loose bowel movements being types 6 and 7.
When there is irritation in the small bowel, it can also be common for there to be malabsorption or maldigestion of fats. This can lead to fatty or greasy-looking stools. [Source: PubMed]
Can you take laxatives if you have methane-SIBO?
For many people with methane SIBO, (IMO) can experience constipation. Not only can constipation lead to pain and discomfort, but it can also increase gas and bloating. To help improve symptoms laxatives and stool softeners can be considered.
While these do not treat the underlying issue, they can help in the short-medium term while the underlying issue is addressed.
One stool softener that is commonly suggested is lactulose. While this may be helpful to a wide number of patients with constipation, lactulose is also classed as a prebiotic. This means that in some, it can increase gas and bloating. [Source: PubMed]
A natural supplement to help with improving constipation in magnesium oxide. This form of magnesium is poorly absorbed and draws fluid into the bowel, introducing more moisture to the stool, thus supporting bowel movements. [Source: PubMed]
What is the best probiotic for SIBO constipation?
When selecting probiotics for digestive issues, it’s important to consider the specific strain of bacteria and what it has been researched for.
For many strains of bacteria, research has found that they can help with IBS symptoms such as bloating or abdominal pain.
There are other strains of probiotic bacteria that have been found to reduce levels of methane in the gut and improve constipation.
The most well-researched strain to do this is a specific strain of Lactobacillus bacteria known as Lactobacillus reuteri DSM 17938. A study from 2017 found that a 4-week treatment course of this probiotic led to a reduction in methane levels which the authors concluded was the reason why constipation and bowel movements improved. [Source: PubMed]
Are bananas OK for SIBO?
For many people with symptoms of IBS and SIBO, a lower-fibre diet can help to reduce and manage symptoms. This type of diet is referred to as a low FODMAP diet.
While this diet may not treat the underlying issue in the gut, removing or reducing these fibres can take a certain amount of strain off the gut and improve symptoms.
As bananas ripen, the balance of sugars and carbohydrates changes. This means that while an unripe banana is low FODMAP, the riper it gets, the more the levels of FODMAP increase. However, if ripe bananas can be eaten without there being an increase in symptoms, they can be included in the diet to avoid the range of foods being needlessly restricted.
A low FODMAP diet should, however be carried out with supervision to guide the elimination and reintroduction process. [Source: PubMed]
Can you gain weight from constipation with SIBO?
When it comes to weight gain and constipation, a confusing factor can be the amount of extra weight that might be coming from the stool remaining in the colon. In addition to this, bloating and distention can also be experienced, this extra gas may give the impression of more weight or body mass, but it may be related to the inflation on the abdomen rather than an actual change in body composition.
Often people with SIBO who have malabsorption and diarrhoea can find that they experience weight loss. This can be due to fewer calories being consumed as well as the fear of food reactions, leading to less food being eaten. [Source: PubMed]
It has also been found that those who are overweight or obese are twice as likely to develop SIBO. This doesn’t mean that being overweight itself causes SIBO. [Source: PubMed]
Is yoghurt good for SIBO?
While dairy products that contain lactose, such as milk, may not be well tolerated by many with IBS and SIBO, yoghurt may be very well tolerated. This is because most of the lactose is digested by bacteria during the fermentation process. [Source: PubMed]
Fermented vegetables have also been well studied in their relationship to gut health and improving gut symptoms. Fermented vegetables such as sauerkraut and kimchi have been researched and found to improve the gut environment by:
- reducing the pH in the gut
- supporting the immune system
- supporting the growth of beneficial bacteria
- inhibiting pathogenic bacteria [Source: PubMed]
While many of the studies have not investigated SIBO directly, we do know that up to 80% of those with IBS may have SIBO as their underlying issue. Therefore we may be able to say with some certainty that if an approach helps with IBS symptoms, it is likely addressing a bacteria overgrowth also. [Source: PubMed]
Can I eat eggs with SIBO?
Eggs are a good source of protein and gut-friendly nutrients such as vitamin D and vitamin A, both of which support the immune response along the lining of the gut. [Source: PubMed]
Due to eggs being low in fibre, they are generally very well tolerated by many people with IBS and SIBO. This food is featured heavily in recipes for both the Low FODMAP diet and the SIBO/Bi-phasic diet. [Source: PubMed]
Conclusion
While certain foods may increase symptoms of bloating if SIBO is present, avoiding those foods won’t address the underlying issue in the gut.
Working to address an underlying imbalance is a central way to both resolve symptoms and then be able to reintroduce any foods being avoided.
We often talk to our patients about the fact we don’t want to spend too much time trying to find out what foods are triggering symptoms, but instead work to address the reason why the gut is behaving in this way.






