
Introduction
A colonoscopy is a procedure that allows your doctor to examine your intestine, rectum, and colon using a long, flexible tube with a camera on the end.
In most cases, mild pain and cramping are experienced by patients during the procedure, but most of them describe it as similar to passing gas or diarrhoea.
It’s also possible for painkillers or sedatives to be prescribed, which can reduce any discomfort. [Source: NHS]
During this procedure, tissue samples (biopsies) are taken to assess for changes in the gut lining that can help diagnose a condition. [Source: Mayo Clinic]
How painful is the colonoscopy procedure?
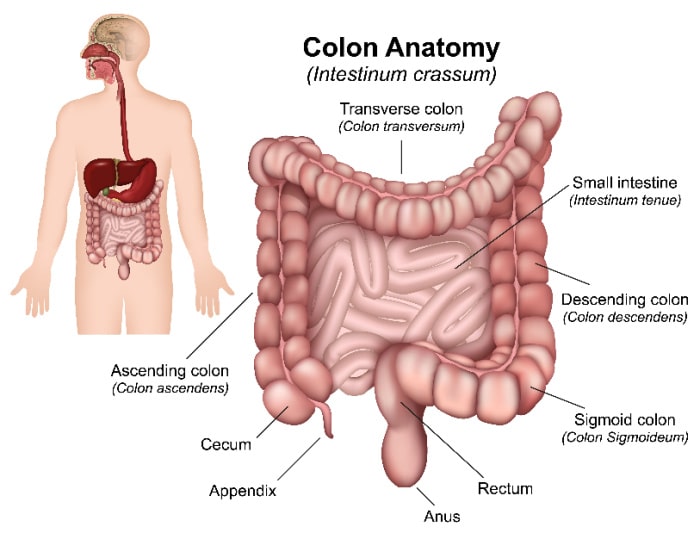
During a colonoscopy, a thin tube is inserted through your rectum and into your colon (large intestine).
This tube has a tiny camera on its tip that lets the doctor see inside as they go along. A small amount of air may be injected into your rectum to help move things along during the exam.
For many, this test is not painful, while for others, due to increased sensitivity in their gut, pain can be felt. If this is the case, sedation may be administered to both reduce pain and to help you relax during the procedure.
Is colonoscopy painful without sedation?
Colonoscopy does not require sedation. The test involves putting a tiny tube into your rectum, so there may be some discomfort, but it is usually not painful.
If you are anxious about the procedure, speak with the doctors about sedation being an option. Additionally, if you are suffering from severe pain, this may also be an important conversation to have. [Source: Mayo Health]
Does a colonoscopy cause lots of pain?
Pain is caused by the insertion of the endoscope into your rectum. The discomfort lasts for about 30 seconds, but it can be controlled with sedation.
The pain you feel during a colonoscopy is usually caused by irritation of the lining of your colon and rectum. This can happen if there are any tears in these tissues or if they were injured before you had your procedure (for example, by constipation).
Another factor that is common in gut issues is visceral hypersensitivity. This is where the nerves are very sensitive along the gut lining. If this is present, the sensations and pain during the colonoscopy may be increased. [Source: PubMed]
 Is a colonoscopy painful?
Is a colonoscopy painful?
A colonoscopy is a common screening test for colorectal cancer, and it’s recommended for people over 50 years old. The procedure can be uncomfortable, but it’s not painful.
It can be an important test to assess bowel health and look for signs of:
- Bowel cancer
- Inflammation bowel disease
- Diverticulitis
- Haemorrhoids
- Polyps [Source: NHS]
Does a colonoscopy hurt if you have haemorrhoids?
If you have haemorrhoids, a colonoscopy may be painful. Haemorrhoids are swollen veins in the rectum or anus that can cause pain and bleeding. A colonoscopy is an invasive medical procedure that allows doctors to look inside your digestive tract for signs of cancer or other diseases by passing a tube through your anus into your colon (large intestine).
If you have haemorrhoids during this process, it can increase discomfort because they make it harder for blood vessels to expand as needed during the insertion of the endoscope (colonoscope). [Source: PubMed]
What causes severe pain during colonoscopy?
While the procedure may often be uncomfortable, it is not always painful. During a colonoscopy, you’ll feel pressure as the tube is inserted into your anus. However, pain may be more present if the gut is already irritated or inflamed.
Air may be pumped into your colon to expand it so doctors can see more clearly during the procedure. This can cause some mild discomfort and bloating afterward, but it shouldn’t be painful unless there are other issues going on with your digestive tract (such as haemorrhoids). [Source: PubMed]
What are the signs of needing a colonoscopy?
There are several signs that indicate you may need a colonoscopy.
These include:
- Trouble with bowel movements and constipation
- A sudden change in bowel patterns
- Blood in stool (the colour of the blood can vary from bright red to black)
- Unexplained weight loss or abdominal pain [Source: Cleveland Clinic]
How long does a colonoscopy take?
A colonoscopy is a procedure that can last anywhere from 30 minutes to an hour.
Sigmoidoscopy, which is similar to colonoscopy but shorter and less comprehensive, takes about 10 minutes. [Source: PubMed]
Endoscopy involves inserting an instrument into your mouth and down to your stomach that has a light and camera on it so doctors can see inside your digestive tract. This type of examination generally lasts 15-20 minutes. [Source: NHS]
Why would you have a sigmoidoscopy instead of a colonoscopy?
A sigmoidoscopy is a shorter and less invasive test than a colonoscopy. It allows doctors to look at the lower part of your colon, which is called the sigmoid. A colonoscopy allows your doctor to examine all parts of your large intestine (colon), including the rectum and anus. [Source: PubMed]
A sigmoidoscopy takes about 15 minutes on average, while a colonoscopy takes around 45 minutes to an hour, depending on how much time the procedure takes. [Source: PubMed]
What does a colonoscopy test for?
A colonoscopy is a test to look at and examine the inside of your colon. Colonoscopy is used to detect polyps and other abnormalities in the lining of your large intestine (colon). It can also diagnose inflammatory bowel disease, such as Ulcerative colitis; it may be used along with biopsies or endoscopic ultrasound (EUS) for diagnosis.
A doctor will insert an instrument called a scope into your rectum so that he can see inside your rectum and lower part of your colon on a video screen. The scope has lenses on each end that allow him to see inside these areas clearly so that he can remove abnormal tissue if necessary or take samples for lab tests if needed. [Source: NHS]
What diseases can be detected by a colonoscopy?
A colonoscopy can detect colorectal cancer, polyps, and other conditions in the large intestine.
Colorectal cancer is one of the most common cancers in men and women. It starts in the colon or rectum (lower part of the digestive tract). A colonoscopy can find early-stage colorectal cancer before symptoms appear when treatment is most likely to be successful.
Polyps are growths that are caused by inflammation of your digestive tract lining or a genetic condition called polyposis syndrome. They’re often spotted during a regular screening exam with no symptoms at all; if left untreated, they can become cancerous. [Source: Cancer]
Haemorrhoids are also known as piles or varicose veins around your anus or lower rectum area. These painful lumps occur when blood vessels inside those areas swell up due to straining during bowel movements or pregnancy hormones that weaken connective tissue holding them in place (haemorrhoids). [Source: NHS]
What are the most common findings of a colonoscopy?
A colonoscopy is the most accurate test for colorectal cancer. During a colonoscopy, your doctor will look for polyps and inflammation in the lining of your colon and rectum.
Biopsies will also be taken to assess for low-level inflammation, such as in microscopic colitis. [Source: PubMed]
Polyps can be removed or left alone depending on their size, shape, and location within your digestive tract.
Inflammation may require medication to reduce symptoms such as abdominal pain or diarrhoea. Further medical intervention will be recommended if cancerous lesions are found during a colonoscopy. [Source: NHS]
Conclusion
A colonoscopy is a procedure that can help diagnose and treat diseases of the colon and rectum. It is recommended for people who are 50 years or older and have had symptoms such as bleeding or changes in bowel habits.
A colonoscopy allows doctors to look at the lining of your intestines through a thin tube inserted into the anus while they are sedated by IV medication. The procedure itself does not hurt, but there may be some discomfort during preparation before surgery.
For many that we see with IBS, they have already had a colonoscopy, which has ruled out many possible causes. However, for IBS, there is a great deal more that can be considered to identify and address the cause of the symptoms.

 Is a colonoscopy painful?
Is a colonoscopy painful?




