
What is endometriosis?
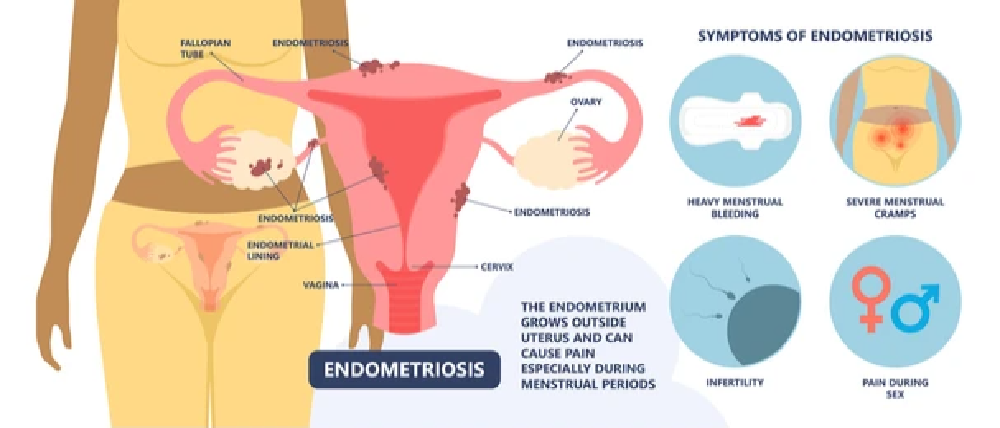
Endometriosis is an inflammatory, oestrogen-dependent condition. It is defined as the presence of endometrial tissues outside of the uterus. This can result in symptoms associated with menstruation, chronic pelvic pain, subfertility as well as digestive symptoms.
While there is no clear understanding of what causes endometriosis there are several theories about its development.
These factors include:
- Retrograde menstrual flow
- Hormonal imbalances
- Inflammation
- Immunological imbalances
Endometriosis can impact 10-15% of women during reproductive age with several symptoms [Source: Pubmed].
What are the symptoms of endometriosis?
The majority of women who are later diagnosed with endometriosis say that their symptoms started in adolescence. These symptoms can vary from woman to woman, but common symptoms are often present in those with endometriosis.
Symptoms of endometriosis include:
- Bleeding partway through the menstrual cycle (intermenstrual bleeding)
- Painful periods (dysmenorrhea)
- Painful intercourse (dyspareunia)
- Painful defecation (dyschezia)
- Painful urination (dysuria) [Source: Pubmed]
It is also very common for there to be a delay in the diagnosis of endometriosis. A 2011 study reported that there is an average delay in diagnosis of endometriosis of 6.7 years [Source: Pubmed]
Reasons for this delay in diagnosis can include the expensive nature of testing for endometriosis. It’s also common for symptoms to alter based on the patient’s menstrual cycle which can make the exact nature of symptoms less clear [Source: Pubmed]
It has been reported that endometriosis can be present in 70% of women with chronic pelvic pain [Source: Pubmed]
What causes endometriosis?
Studies have reported several factors associated with the reproductive system that are associated with endometriosis. This highlights the possibility of hormonal changes influencing the risk of endometriosis developing.
The hormonal factors that may increase the risk of developing endometriosis include an earlier age when the menstrual cycle first started as well as a shorter duration of the menstrual cycle. It has also been noted that the current use of oral contraceptives and the number of times a woman has given birth (the risk decreases and births increase) carry a decreased risk [Source: Pubmed]
While smoking has been linked to many health issues, several studies have interestingly associated it with a decreased risk of endometriosis. This was particularly true if the developing foetus was exposed to cigarette smoke. In this case, an 80% reduced sick of endometriosis was found. However, in contrast to this, passive smoking during childhood increases the risk of developing endometriosis.
The exact reason for this is not known. However, one theory is that smoking reduced circulating oestrogens which could reduce the growth of endometrial tissue [Source: Pubmed]
Inflammation and Endometriosis
Certain dietary patterns may also contribute to an increased risk of endometriosis. In particular the intake of omega-3 fatty acids.
A 2010 study reported that the women with the highest intake of these fats were 22% less likely to be diagnosed with endometriosis. In contrast, those with the highest intake of trans-fats (often present in processed and fried foods) were at a 48% increased risk of developing endometriosis.
These beneficial fats are found in foods such as:
- Salmon
- Herring
- Mackerel
- Sardines
- Flaxseeds
- Chia seeds [Source: Pubmed]
Also Read: What Helps Endo Belly?
How is Endometriosis diagnosed?

While several tests can be carried out to offer a preliminary diagnosis of endometriosis, the gold standard (the best test) is a laparoscopic inspection. This test will also remove a small amount of endometrial tissue which is then examined further [Source: Pubmed]
As mentioned, pelvic pain is a symptom of endometriosis, however, there are other conditions that cause pelvic pain. It’s not uncommon for these to be ruled out ahead of a laparoscopy.
These tests include:
- Urinalysis
- Pap smear
- Pregnancy test
- Vaginal and endocervical swabs.
Ultrasounds can also be used as a preliminary test with pelvic masses best viewed via a transvaginal or transabdominal ultrasound. There are differences between these 2 types of ultrasound procedures.
A transvaginal ultrasound offers a clearer view of the endometrium and the uterine cavity. This can help to view ovarian endometriotic cysts, but this doesn’t rule out endometriosis in the peritoneal cavity, adhesions associated with endometriosis or deep infiltrating endometriosis [Source: Pubmed]
Alterations in the results of certain blood tests are commonly seen in women with endometriosis. These include alterations in the levels of CA-125, cytokines and growth factors. However, these are not reliable enough to be used as a diagnostic tool for endometriosis [Source: Pubmed]
Can endometriosis cause IBS?
Endometriosis can lead to the gynaecological symptoms previously mentioned in this article. It has also been found that digestive issues are extremely common in women with endometriosis.
Gastrointestinal symptoms impact up to 90% of those with endometriosis. The most common gut symptom found with endometriosis is bloating but additional symptoms are often present. These include:
- Nausea
- Constipation
- Diarrhoea
- Vomiting [Source: Pubmed]
Also Read: Endometriosis & IBS – What’s The Connection?
Endometriosis and the gut bacteria
The gut bacteria are also referred to as the gut microbiome. This is a complex ecosystem that contains a wide range of microorganisms which include, bacteria, viruses, archaea and yeasts.
This organism aid in food digestion, immune regulation and metabolism. This not only impacts gut function but overall well-being.
It’s been seen that the gut microbiome is less diverse in those with endometriosis when compared to healthy controls. Since diversity (the range of organisms in the gut) is a key indicator of how healthy the gut is, a less diverse gut microbiome is considered less healthy [Source: Pubmed]
Endometriosis also appears to be associated with increases in certain groups of bacteria associated with inflammation. These include:
- Proteobacteria [Source: Wiley]
- Enterobacteriaceae [Source: Pubmed]
- Streptococcus [Source: Nature]
- Escherichia coli [Source: Pubmed]
It is also well-reported that changes in levels of oestrogen impact the gut microbiome. This can be one link between the hormonal changes found in endometriosis and imbalances in gut bacteria. It is also known the gut microbiome can impact oestrogen levels. This means that the gut microbiome can be involved in the development of endometriosis, but endometriosis and the way it is treated may further impact the gut microbiome [Source: Pubmed]
Animal studies have shown that antibiotic usage can reduce the progression of endometriosis however, this has not been studied in humans [Source: BMJ]
The Gut Microbiome and Oestrogen
Within the gut microbiome, there are certain bacteria with specific genes that impact oestrogen levels. This has been termed the ‘estrobolome’.
Certain bacteria produce an enzyme called beta-glucuronidase which may increase how much oestrogen is reabsorbed from the gut into circulation. Therefore higher levels of -beta-glucuronidase in the gut may lead to high levels of circulating oestrogen
The understanding here is that an imbalanced but can produce more beta-glucuronidase. This then leads to more oestrogen being reabsorbed into circulation which has the potential to promote the development and progression of endometriosis [Source: Pubmed].
Conclusion
Once diagnosed, the gut is a central focus when addressing the imbalances seen in endometriosis. This is due to the importance of the gut in:
- Hormonal balance [Source: Pubmed]
- Detoxification [Source: Pubmed]
- Balancing inflammation
- The immune response [Source: BMC]
Working with a Registered Nutritional Therapist can guide you through this process and support the above via personalised dietary recommendations, appropriate supplements and further testing.






