IBS (Irritable Bowel Syndrome)
We can help you identify and address the underlying cause of your gut issues so you can live a symptom-free life.
Your IBS Symptoms
Have you had several tests carried out by a doctor or gastroenterologist but everything is clear? The common next step is that you've been diagnosed with IBS.
Are your symptoms ruling your life?
IBS can impact the quality of life. Leading to fear of foods, missing social engagements and urgent trips to the toilet.
Are you looking for an answer?
Not knowing the cause of your symptoms can lead you to spend a lot of time on Google. Often this only adds more confusion.


What is IBS?
IBS (Irritable bowel syndrome) is a common digestive condition which can significantly impact quality of life.
This means that effective treatment and management are important.
The common symptoms of IBS include:
- Bloating and distention
- Abdominal pain and cramps
- Changes in bowel patterns (eg. constipation or diarrhoea)
- Food intolerances
What are the types of IBS?
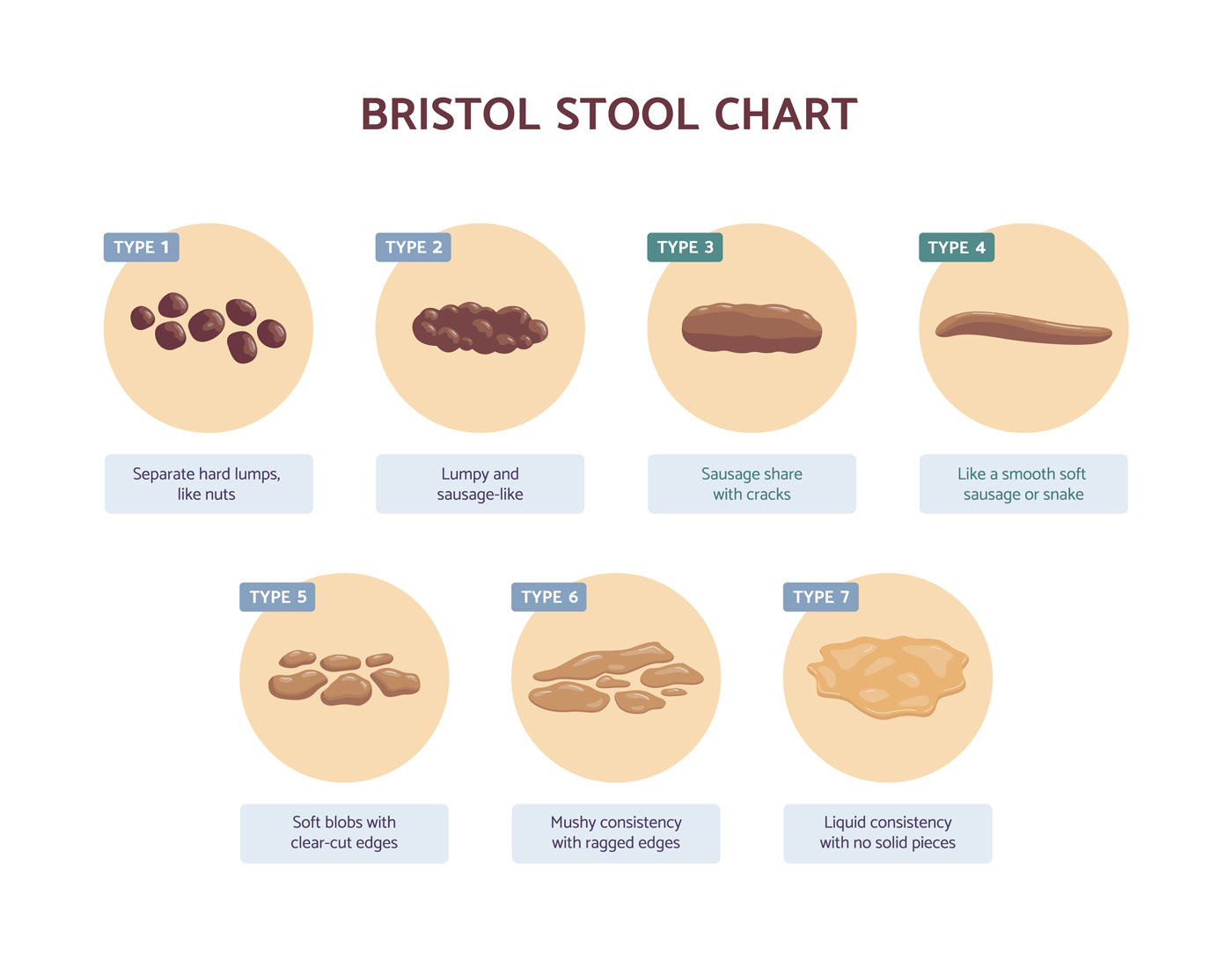
Symptoms such as pain and alterations in bowel patterns are required for a diagnosis of IBS. It’s also possible to diagnose and categorise IBS by subtype.
This is related to the types of bowel movements being experienced.
The IBS subtypes are:
- IBS-C (IBS with constipation) – requires at least 25% of bowel movements to be with type 1 or type 2.
- IBS-D (IBS with diarrhoea) – requires at least 25% of bowel movements to be type 6 to type 7.
- IBS-M (IBS with mixed stool form)
- IBS-U (IBS with unclassified stool form)
What are the causes of IBS?
Dysbiosis
Alterations in the balance of the gut microbiome can lead to bloating, cramping, constipation, diarrhoea as well as food intolerances.
These imbalances may be in the small or large intestine and can be caused by factors such as long-term dietary patterns or the use of antibiotics.
SIBO (Small Intestinal Bacterial Overgrowth)
SIBO refers to an overgrowth of bacteria in the small intestine. This can be one of the main causes of IBS symptoms.
Risk factors for developing SIBO include food poisoning, gastroenteritis, the use of certain medications as well as thyroid issues.
Food Poisoning & Gastroenteritis
Events of food poisoning, travellers’ diarrhoea and gastroenteritis can increase the risk of developing IBS by 600% over the following 2-3 years (1).
This can be due to an ongoing low-level inflammatory response within the gut wall that contributes to the ongoing nature of IBS symptoms.
IBS that started this way is referred to as post-infectious IBS.
Food Intolerances
It is possible for food reactions to be the result of changes in the gut microbiome or an overactive immune response.
Assessing how you are responding to foods can help us personalise your treatment plan.
Visceral Hypersensitivity
Increased nerve sensitivity along the lining of the digestive tract can be responsible for specific IBS symptoms.
This can include pain, discomfort and the sensation of increased pressure in the abdomen.
Gut-brain Connection
Increased levels of stress or strain on the central nervous system may impact digestive health and function.
Even once this stress has resolved, symptoms may continue that we can work to address.
Underlying Causes
Underlying imbalances in the gut can lead to the symptoms of IBS. While symptom management strategies can be important, our aim is to resolve the underlying issue.
Personalised Treatment
Our comprehensive intake process assesses the underlying factors that are contributing to your symptoms. From this, we create a personalised treatment plan for you to follow.
Ongoing Support
Our consultations also include regular support and monitoring of your symptoms. This allows us to review your response and make relevant adjustments to the treatment plan.
IBS Treatments
When addressing IBS, the aim is not to simply manage symptoms but to address the underlying factors that are leading to symptoms.
The can require a personalised treatment approach that includes:
- Dietary analysis and support
- Evidence-based gut health supplements
- Lifestyle support
- Gut health tests
- Gut-brain support

Speak to us about your gut health today
What are the symptoms of IBS?
Specific symptoms are required for a diagnosis of IBS. These are outlined in the ROME criteria which state that for a diagnosis of IBS:
Recurrent abdominal pain on average at least 1 day/week in the last 3 months, associated with two or more of the following criteria:
- Related to defecation
- Associated with a change in the frequency of stool
- Associated with a change in form (appearance) of stool
These criteria for IBS can help to provide guidelines for the symptoms of IBS and diagnosis.
While this can be important, the aim of the approach that we take is to go address the reason why symptoms are present.
How is IBS diagnosed?
IBS is often considered a diagnosis of exclusion. This can mean that an IBS diagnosis is made once other conditions have been ruled out.
Before IBS is diagnosed, the following conditions may be tested for:
- Coeliac disease
- Inflammatory bowel disease
- Bowel cancer
While ruling out these other conditions is often important, negative test results can result in uncertainty about the actual cause.
Our approach is to dig deeper to understand and address the underlying reason for your symptoms.
Frequently asked IBS questions
Are supplements needed to address IBS?
We consider the use of a range of evidence-based supplements to address the root causes of symptoms which include:
- Probiotics
- Prebiotics
- Herbal formulas
- Gut lining support
Are elimination diets long-term?
One approach to identifying food triggers and management symptoms is a short-term elimination diet, such as the Low FODMAP diet. However, elimination diets serve short-term dietary strategies to manage symptoms, not as a permanent dietary solution.
Once the underlying issue is addressed, the aim is for the diet to be diverse and relaxed.

Martin Cohen – Dip CNM, CNHC, BANT
Registered Nutritional Therapist, Clinic Director
Client Conversations
Conversations with those we’ve already helped.
Rebecca
Rebecca’s symptoms of IBS started after taking antibiotics for tonsillitis. She cut out foods and introduced supplements by herself, but her symptoms continued.
With our support, Rebecca is now symptom-free.
Geri
Geri’s gut issues started decades ago. After several trips to her GP, treatment for H Pylori and even the removal of her gallbladder she was still experiencing symptoms.
Since working with us, Geri’s symptoms have stopped.
Stella
Stella’s digestive problems started gradually. This led her to cut foods one at a time and survive on an increasingly restrictive and bland diet. Even with doing this, she was still experiencing symptoms.
Stella can now eat a varied diet without experiencing gut issues.



Martin Cohen Dip CNM, mBANT, mCNHC
Registered Nutritional Therapist
Getting help with IBS
The IBS & Gut Health Clinic provides the personalised support needed to identify and address the underlying causes of symptoms.
The support is carried out over a series of consultations to create a personalised strategy to address the root cause.
This will include detailed dietary suggestions, a supplement protocol, recommendations for further testing as well and appropriate lifestyle recommendations.
Your Next Step
Learn about our consultations
Follow the link to learn more about our consultations and how we can support you.
Read more about symptoms and causes
Understand the symptoms and causes of IBS and how they could be impacting you.

